Advance care planning is really just the process of thinking about, talking about, and writing down your wishes for future healthcare. Think of it as creating a personal 'healthcare roadmap' for your family and doctors to follow if you're ever unable to speak for yourself. It’s all about making sure your values guide your care, no matter what.
Your Voice in Future Healthcare

Imagine for a moment that a sudden illness or accident left you unable to communicate. Who would make medical decisions for you? What would they say?
Answering these tough questions now, while you’re able to think clearly, is the whole point of advance care planning. It's not a one-and-done document; it's a thoughtful process.
This kind of planning puts you in the driver's seat, reducing a lot of future stress and confusion for the people you love. By clearly stating your wishes, you give them the incredible gift of clarity. You relieve them of the heavy burden of guessing what you would have wanted during an already emotional time.
Why Planning Matters Now More Than Ever
Having clear healthcare directives is becoming more critical every day. In fact, the global market for advance directives—a key part of this planning—was valued at US$122.74 billion in 2023. It’s projected to skyrocket to US$588.40 billion by 2032.
This massive growth shows a real shift in awareness, driven by our aging population and new medical technologies. You can explore the data behind this trend in this detailed market report on advance directives.
Advance care planning is one of the most proactive and compassionate steps you can take for your family. It ensures your voice is heard, your dignity is protected, and your loved ones are supported when they need it most.
The Core Goals of Planning Ahead
At the end of the day, this process is all about making sure the medical care you receive lines up with your personal values, beliefs, and what you consider a good quality of life.
It boils down to three main goals:
- Choose a healthcare agent (sometimes called a proxy or representative) to make decisions for you if you can't.
- Document your preferences about specific medical treatments you would or would not want.
- Share your plan with your family, your agent, and your doctors so everyone is on the same page.
By defining what matters most to you, you provide a clear, invaluable guide for everyone involved in your care.
The Key Documents in Your Healthcare Roadmap
While advance care planning starts with a conversation, it eventually leads to putting those wishes down on paper. These legal documents are the official instructions in your healthcare roadmap, making sure your voice is heard and legally recognized when it matters most.
These papers are formally known as advance directives. Think of them as the foundation of your plan. Let's break down the most common ones so you can feel confident building a complete and effective plan.
The Living Will: Your Instruction Manual
A Living Will is a written statement that details the kind of medical treatments you would—or would not—want if you are ever permanently unconscious or terminally ill. It’s your direct instruction manual for your medical team when you can't speak for yourself.
For instance, your Living Will can spell out your wishes on:
- Life-Sustaining Treatments: This includes things like mechanical ventilation (breathing machines) or tube feeding.
- Palliative Care: You can direct your team to focus on comfort and pain management rather than treatments aimed at a cure.
This document ensures your personal values about quality of life are respected, even when you're unable to communicate them.
The Durable Power of Attorney for Healthcare: Your Trusted Advocate
While a Living Will outlines what you want, the Durable Power of Attorney for Healthcare (DPOAHC) names who will make decisions for you. This person is often called a healthcare agent or proxy, and they are empowered to make medical choices on your behalf if you become incapacitated.
This role is absolutely vital because no document can predict every possible medical situation. Your agent acts as your advocate, interpreting your wishes and making judgments in real-time based on the values you've shared. It's important to understand how these documents work together, and you can learn more by exploring resources that compare a Living Will vs. Power of Attorney.
Choosing the right person is a huge part of advance care planning. For more detailed guidance on selecting your advocate, check out our article on medical and financial power of attorney forms.
The POLST Form: A Medical Order for the Seriously Ill
A POLST, which stands for Practitioner Orders for Life-Sustaining Treatment, is very different from an advance directive. It's an actual medical order, signed by your doctor, that translates your wishes into actionable instructions for first responders and other healthcare providers.
A POLST is only for individuals with a serious illness or advanced frailty. Unlike a Living Will, it goes into effect the moment it's signed and travels with you across different care settings—from home to the hospital and back again.
A POLST essentially turns your personal wishes into a direct medical order. In New Jersey, it's printed on bright pink paper so emergency personnel can recognize it immediately, ensuring your end-of-life choices are honored in a crisis.
To help clear up any confusion, it's helpful to see these two documents side-by-side.
Living Will vs. POLST: Understanding the Difference
| Feature | Living Will (Advance Directive) | POLST Form |
|---|---|---|
| Who It's For | Any adult, regardless of health status. | Individuals with a serious illness or advanced frailty. |
| What It Is | A legal document stating future care preferences. | A medical order signed by a doctor. |
| When It's Used | Only if you are unable to make your own decisions. | Effective immediately upon being signed. |
| Purpose | Guides your healthcare agent and doctors on your wishes. | Gives direct instructions to all medical personnel. |
Understanding the distinction is crucial. A Living Will states your wishes for the future, while a POLST is a current medical order for a specific health condition that requires immediate action.
Why This Conversation Matters for Every Adult
It’s a common myth that advance care planning is only for the elderly or people with a serious illness. The truth is, life is unpredictable. A sudden accident or health crisis can happen to anyone at any age, leaving them unable to communicate their own wishes for their care.
This is exactly why this conversation is so important for every adult. This isn't about planning for the end of life; it's about being prepared for the unexpected. It’s about making sure your values and personal dignity are always front and center, no matter what happens.
Without a plan, the weight of making difficult, often heart-wrenching medical decisions falls squarely on your family's shoulders. They’re left guessing what you would have wanted, which can breed stress, guilt, and even painful conflict during an already emotional time.
A Proactive and Compassionate Act
Thinking through your wishes isn't just a practical to-do item; it's a profoundly compassionate act for the people you love. You're giving them the gift of clarity and peace of mind. Instead of facing paralyzing uncertainty, your family and doctors have a clear roadmap to follow, ensuring the care you get is exactly what you would have chosen.
This process gives you the power to:
- Maintain Control: You stay in the driver's seat of your own medical care, even when you can't speak for yourself.
- Prevent Family Conflict: A clear, written plan removes the burden of guesswork and helps avoid disagreements among loved ones.
- Ensure Dignity: Your personal beliefs about what makes life meaningful are honored, protecting your dignity throughout your entire care journey.
Despite these obvious benefits, a surprising number of adults haven't taken these steps. A comprehensive study across 11 high-income nations found that only 27.4% of older adults had completed all the key activities. Here in the U.S., where end-of-life healthcare costs can be a major stressor, proper planning can reduce hospitalizations and ease both the financial and emotional load on families. You can read the full study about advance care planning completion rates.
This isn't just about filling out forms. It's about having thoughtful conversations that protect you and the people you love from facing a crisis without a map. It’s an act of love.
A critical piece of this puzzle is choosing someone to speak on your behalf, often called a healthcare agent or proxy. It's vital to understand how this role is different from other legal appointments. For a deeper dive into these distinctions, you might find our guide on the difference between guardianship and power of attorney helpful.
How to Start Your Advance Care Plan
Thinking about advance care planning can feel overwhelming, but it doesn't have to be. The key is to break it down into small, practical steps. Think of it as a journey in four parts, starting with some quiet reflection and ending with a clear, legally sound plan.
We'll walk you through each phase, from figuring out your own values to signing the final papers, so you can start the process with confidence.
Step 1: Reflect on Your Values and Wishes
The heart of any good advance care plan is you—your beliefs, what you value, and what a good quality of life means to you. Before you can explain your wishes to anyone else, you have to be clear on them yourself. This first step is all about looking inward.
Take some time to really think about these kinds of questions:
- What are the things that bring you joy and make your life feel meaningful?
- If you were facing a serious illness, would your priority be living as long as possible, or would you focus more on comfort and quality of life?
- Are there specific medical interventions, like being on a ventilator or a feeding tube, that you would want to avoid in certain situations?
Jotting down your thoughts can make them feel more concrete and prepare you for the conversations ahead with family and doctors.
Step 2: Choose Your Healthcare Representative
One of the most important decisions you'll make in this process is choosing your healthcare representative (sometimes called an agent or proxy). This is the person you trust to make medical decisions on your behalf if you ever become unable to speak for yourself.
Your healthcare representative is more than just a name on a form; they are your voice. Choose someone who understands your values deeply, can handle stress, and will advocate fiercely to ensure your wishes are honored.
When you're thinking about who to choose, consider if they are assertive, calm under pressure, and truly willing to take on this huge responsibility. It’s always a good idea to pick one primary person and at least one alternate, just in case.
Step 3: Have the Conversation
Once you've done your own reflection and picked a representative, it's time to talk. Having open, honest conversations with your family, your chosen representative, and your doctors is absolutely essential. These talks make sure everyone understands your plan and is on the same page.
It doesn't have to be a dramatic announcement. You can start simply by saying something like, "I've been thinking about the future, and it’s really important to me that you know my wishes for my healthcare. Can we find some time to talk about it?"
Step 4: Complete the Necessary Documents
The last step is to make your plan official by filling out the legal forms. In New Jersey, this usually means completing an Advance Directive, which combines a Living Will with the formal appointment of your healthcare representative. If you have a serious illness, your doctor might also suggest a POLST form.
This flowchart shows how planning ahead empowers you, guides your family, and protects your choices.
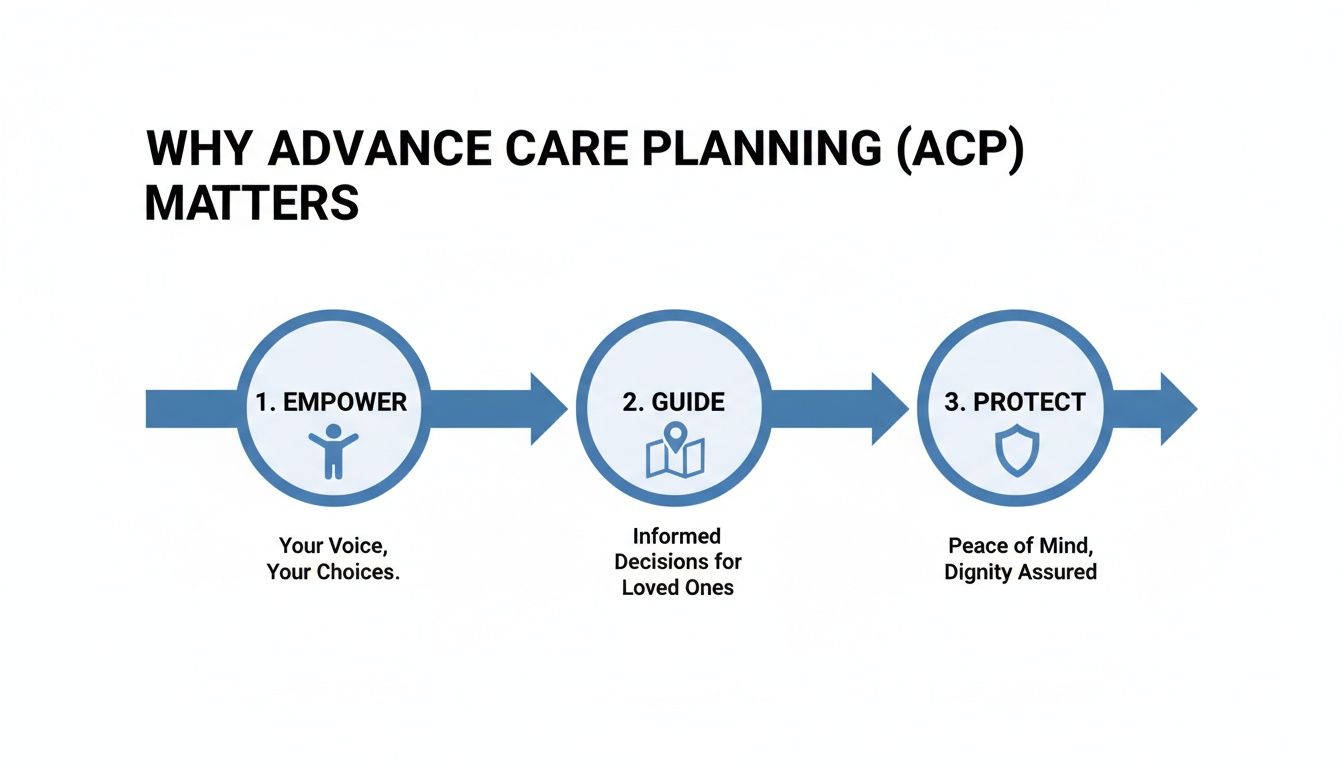
This visual really drives home the core benefits—it starts with you feeling empowered, leads to clear guidance for your loved ones, and ultimately protects your right to make your own healthcare decisions.
Once your documents are finalized, it's critical that the right people can access them when needed. Understanding the rules for HIPAA compliant document sharing protects your privacy while ensuring your healthcare team has the information they need. Make sure to give copies to your representative, key family members, and all of your doctors.
Navigating the Process in New Jersey
While the big ideas behind advance care planning are the same everywhere, the nitty-gritty legal details change from state to state. Here in New Jersey, getting those details right is what makes your healthcare roadmap legally binding and ensures it will be followed by doctors and hospitals.
It really comes down to knowing what makes an advance directive official in the Garden State. For example, a New Jersey Advance Directive has to be signed by you (or by someone else for you, while you're present) and then be witnessed by two adults or a notary public. Following these rules to the letter is what gives the document its power when it matters most.
Finding the Right Forms in New Jersey
To keep things simple, it’s always best to start with state-approved forms. The State of New Jersey provides official documents that already meet all the legal requirements, like the combined Advance Directive for Health Care. This single form is incredibly helpful because it lets you both state your specific wishes (the "living will" part) and name your healthcare representative all in one place.
For anyone managing a serious illness, the New Jersey POLST (Practitioner Orders for Life-Sustaining Treatment) is a different but equally important document. This is a medical order, not just a legal one, that you fill out directly with your doctor. Using these official state resources means your plan will be clear, complete, and recognized in any healthcare setting across New Jersey.
A knowledgeable local partner, like the team at NJ Caregiving, can be an invaluable guide. We help families navigate these state-specific requirements, facilitate tough conversations, and ensure a loved one's care plan aligns perfectly with their documented wishes.
Having this local support is more important than ever. The U.S. market for advance care planning solutions was valued at a massive USD 101.4 billion in 2023. With both Medicare and Medicaid now reimbursing providers for having these conversations, more doctors are starting them with patients, especially those with long-term health conditions.
How a Local Care Partner Helps
Having a partner on the ground who truly understands New Jersey's system can make all the difference. At NJ Caregiving, we’re deeply familiar with the resources and rules right here in Mercer County.
We can point you to the correct forms and help you see how your plan works with other services, like those covered by New Jersey Medicaid waiver programs. Our goal is to give you the clear, practical information you need to create a plan that brings real peace of mind.
Common Questions About Advance Care Planning
It's completely normal to have questions, even after you get the basics down. This whole process touches on some deeply personal topics, and feeling a little hesitant is part of it. Let's clear up some of that uncertainty so you can feel confident moving forward.
We'll tackle the most common questions we hear, bust a few myths, and give you the practical info you need to take that next step.
Do I Need a Lawyer to Create an Advance Directive?
This is one of the biggest myths that stops people in their tracks. The short answer is no, you do not need a lawyer to create a legally valid advance directive in New Jersey. The state actually provides official forms that you can fill out yourself.
The most important part is getting it witnessed correctly. In New Jersey, your completed directive has to be signed in front of either:
- Two adult witnesses
- A notary public
While an attorney can always help, especially if you have a complicated family or financial situation, it’s not required for most people. The system is designed to be accessible.
When Is the Best Time to Start This Process?
The absolute best time to start advance care planning is right now—while you’re healthy and can think things through without pressure. So many people put it off, thinking it’s only for older folks or someone with a serious diagnosis. But the truth is, a medical emergency can happen at any age.
Planning ahead is not about anticipating the end of life; it’s about preparing for the unexpected. Completing your documents when you are in good health ensures your decisions are proactive and thoughtful, not reactive and rushed during a crisis.
Think of it like insurance. You get it hoping you’ll never need it, but there's incredible peace of mind in knowing it’s there. Starting the conversation today is a true gift to your future self and your family.
What Happens If I Change My Mind Later?
Nothing is set in stone. Your life will change, your health will evolve, and what’s important to you might shift over time. Your advance directive is a living document, and you can—and should—update it whenever your wishes change.
You have the right to change or completely cancel your advance directive at any time. All you have to do is complete a new form, making sure it’s properly signed and witnessed just like the first one.
It’s a great idea to review your documents every few years or after a major life event, like:
- A new medical diagnosis
- Getting married or divorced
- The death of a loved one, especially if they were your chosen healthcare representative
Once you create a new directive, it's critical to destroy all the old copies. Then, hand out the new version to your representative and doctors to make sure there's no confusion.
Who Should I Give Copies of My Documents To?
A plan doesn't do much good if it's a secret. Once your advance directive is complete, you need to share it with the key people in your life. Tucking it away in a safe deposit box could make it totally useless in an emergency.
Make sure these people have a copy on hand:
- Your healthcare representative (and any backups you named)
- Your primary care physician and any specialists you see
- Your local hospital (they can add it to your medical records)
- A trusted family member who isn't your representative but should know your wishes
Giving them a physical or digital copy makes sure your plan is ready the moment it's needed, allowing everyone to honor your wishes without delay. It’s the final step to ensuring your voice is heard.
Navigating the details of advance care planning can feel like a lot, but you don't have to figure it all out alone. At NJ Caregiving, our team helps families in Mercer County understand their options, get these important conversations started, and connect with the right resources. If you're ready to create a plan that gives you security and your loved ones clarity, we're here to help. Find out more about our compassionate in-home care services by visiting https://njcaregiving.com.


