Bringing a loved one home after a stroke is a huge moment, and it can feel pretty overwhelming. But the secret to good stroke patient care at home is starting with a calm, organized plan. Those first 72 hours are everything—they set the tone for the entire recovery journey. This isn't about long-term strategy yet; it's about immediate safety, getting the medications right, and creating a comfortable space that actually helps them heal.
Navigating The First 72 Hours After Discharge
That transition from the structured, beeping environment of the hospital back to the quiet of home is a big deal. You're probably feeling a mix of relief and a whole new wave of anxiety. As a caregiver, your main job in these first few days is to stop reacting and start proactively managing. It’s time to turn that stack of discharge papers into real-world actions that make your home safe and stable from the minute you walk in the door.
The hospital team gives you the medical playbook, but you’re the one who has to run the plays on the field. This is more than just swinging by the pharmacy—it’s about creating a solid system. It's not just about getting them home; it’s about making home a true safe harbor for recovery.
And you're not alone in this. The trend toward recovering at home is growing for a simple reason: it works. Over the last couple of decades, there's been a massive shift away from sending stroke survivors to care homes. One UK study actually found that number dropped by a staggering 80% between 1995 and 2018. It just goes to show how much we value the healing power of being in a familiar environment.
Establishing Your Immediate Priorities
In these first few days, your focus needs to be sharp and impactful. Don't try to solve every potential problem for the next six months. Instead, lock in on three core areas that will build a strong foundation.
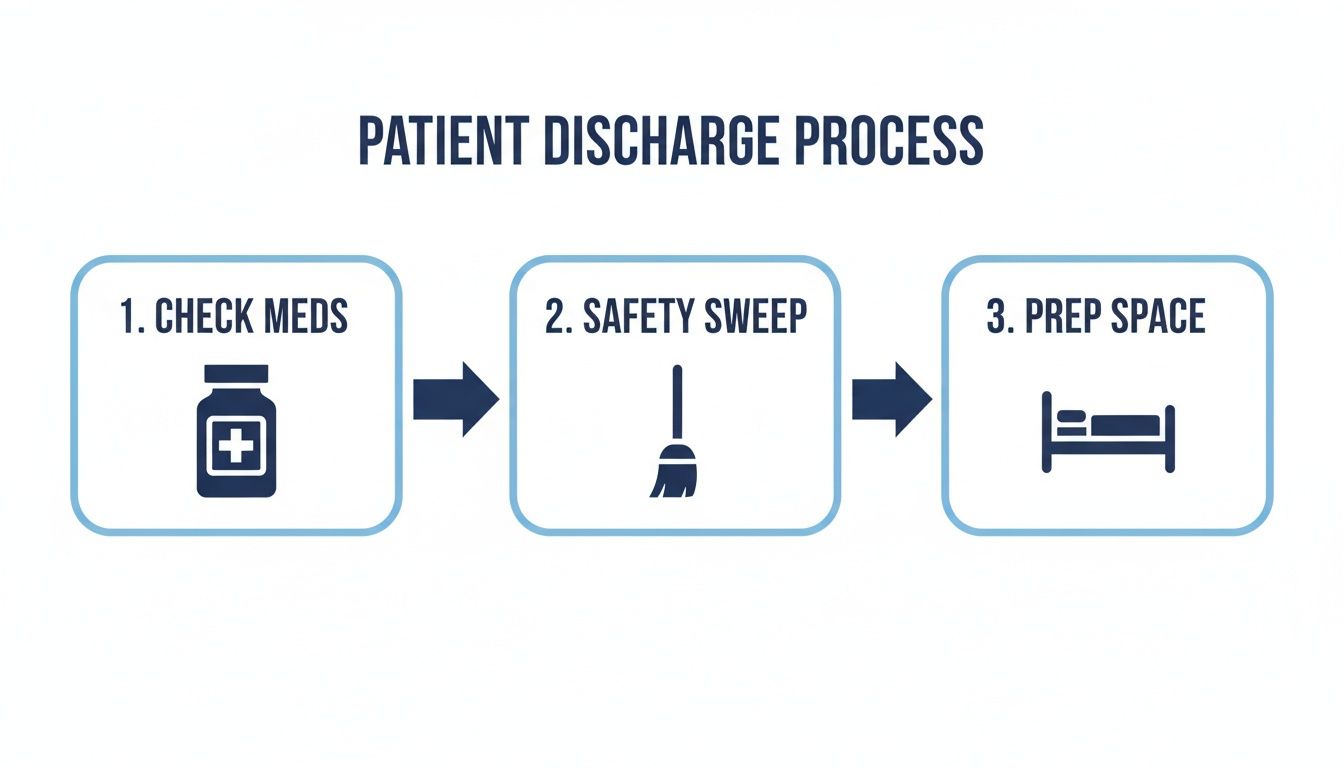
Nailing these three things right away cuts down on immediate risks and brings a sense of order to what can feel like a chaotic time.
First, the meds. As soon as you get them from the pharmacy, sit down with the bottles and the discharge summary. Check that everything matches exactly—the name of the drug, the dosage, how often it’s taken. If anything looks off, don't guess. Call the pharmacist or the doctor's office right away.
Next, do a quick but serious home safety sweep. Your mission is to get rid of any obvious fall hazards before they become a problem.
- Roll up the rugs. All those little throw rugs and runners are major tripping risks. Get them out of the way for now.
- Clear the decks. Make sure there are wide, clear paths to the bathroom, kitchen, and bedroom. No clutter.
- Light the way. Plug in some nightlights in the hallways and bathroom. It makes a huge difference for those middle-of-the-night trips.
Finally, set up a "recovery zone." This might be in the living room or a downstairs bedroom—wherever is most comfortable and accessible. Make sure everything your loved one might need is right within arm's reach: a bottle of water, tissues, the remote, their phone, and a call bell if you have one.
The goal isn’t to turn your home into a hospital room, but to make it a functional, supportive, and safe environment that encourages rest and facilitates care.
To help you stay on track during this critical time, here's a quick checklist of what to focus on.
Immediate Post-Discharge Checklist
This table breaks down the essential tasks for the first few days back home, helping you create a safe and organized environment for recovery.
| Task Category | Action Items | Why It Matters |
|---|---|---|
| Medication Management | Verify all prescriptions against the discharge summary. Organize pills in a daily dispenser. Set alarms for doses. | Prevents dangerous medication errors, which are common during transitions of care. Establishes a crucial routine from day one. |
| Home Safety | Remove throw rugs, clear pathways of clutter, and add nightlights. Check that assistive devices (walker, cane) are properly sized. | Drastically reduces the immediate risk of falls, a leading cause of rehospitalization for stroke survivors. |
| Comfort & Accessibility | Set up a central recovery area with essentials (water, phone, call bell) within easy reach. | Minimizes the need for the patient to strain or move unnecessarily, promoting rest and preventing fatigue or accidents. |
| Communication | Post emergency contacts and the doctor's number in a visible place. Inform key family members of the new routine. | Ensures everyone is on the same page and can act quickly in an emergency, reducing confusion and stress. |
Following these steps methodically can bring a sense of control and confidence as you begin this new chapter.
Having a detailed plan really can make all the difference. For a comprehensive guide to ensure you cover all your bases, check out our helpful discharge planning checklist that outlines every step. This period is also a smart time to think about professional support. An experienced in-home caregiver can step in right away, helping you manage these initial tasks and giving your family invaluable peace of mind.
Mastering Daily Routines and Mobility Support
When your loved one comes home after a stroke, the structured environment of the hospital is replaced by the hands-on reality of daily life. This is where the true work of recovery begins, shifting from clinical schedules to creating new routines at home. It’s about more than just checking off tasks; it’s about rebuilding a sense of normalcy, dignity, and independence when even the simplest activities feel monumental.

The transition can be jarring for everyone. Activities we all take for granted—showering, getting dressed, eating a meal—now demand patience, a new strategy, and often, teamwork. Your goal is to find that delicate balance between providing the help they need and encouraging them to do what they can on their own. This is how you help rebuild their confidence and keep them motivated.
Navigating Activities of Daily Living with Dignity
Assisting with Activities of Daily Living (ADLs) is a mix of practical skill and emotional awareness. Every task is an opportunity to empower your loved one, not just care for them.
Take dressing, for example. Lay out their clothes in the order they’ll be put on. A simple tip is to encourage them to dress their weaker side first, which makes the whole process less physically taxing. Adaptive clothing with Velcro or magnetic closures can be a real game-changer, turning a potentially frustrating ordeal into a moment of success.
Bathing brings its own set of challenges, especially since the bathroom is a high-risk spot for falls.
- Safety First: A shower chair or bench and a handheld showerhead are non-negotiable for stability.
- Encourage Participation: Let them wash themselves as much as they can, even if it’s just with a washcloth while seated. Every bit of independence counts.
- Maintain Warmth and Privacy: Keep the bathroom warm and use towels to cover parts of the body not being washed to preserve their sense of dignity.
The key is to break every task into small, manageable steps. Celebrate the little wins, like buttoning a shirt or combing their own hair. This kind of positive reinforcement is absolutely crucial for their morale.
Ensuring Safe Mobility and Transfers
Getting around the house safely is a top priority. A stroke can wreak havoc on balance, strength, and coordination, making transfers—moving from a bed to a chair, for instance—a critical skill to master. Doing it wrong can lead to serious injury for both of you.
Always tell them what you're about to do before you start moving. Slow and deliberate is the way to go. If they use a walker or cane, make sure it’s always within reach and that they’re using it correctly, putting weight on their stronger side.
Safe transfers are more about technique than brute strength. To move from a bed to a wheelchair, bring the chair close to the bed at a 45-degree angle and lock the brakes. Help them pivot on their stronger leg, using a gait belt around their waist for a secure grip. For a detailed walkthrough of different methods, you can explore our guide on wheelchair transfer techniques (https://njcaregiving.com/wheelchair-transfer-techniques/), which provides step-by-step instructions for a variety of situations.
Establishing Predictable and Supportive Routines
Structure and predictability are incredibly comforting for a stroke survivor. Since cognitive and emotional changes are common after a stroke, a consistent daily schedule can reduce a lot of anxiety by providing a familiar framework for the day.
Try to keep meals, medication, therapy exercises, and rest periods at the same time each day. A simple whiteboard with the day's schedule can be a great visual reminder, giving them a sense of control and awareness.
Remember, recovery is not a straight line; there will be good days and bad days. Frustration and even resistance are normal parts of the process. On tough days, meet them with compassion, not pressure. Sometimes the best support you can offer is just your patience and understanding. A professional caregiver can be an invaluable partner on this journey, providing not just the physical help with ADLs and mobility, but also the gentle encouragement needed to get through the emotional highs and lows.
Managing Medications, Nutrition, and Complications

Once your loved one is home after a stroke, the focus of care shifts dramatically. The daily mission becomes preventing a second event and managing their overall health. This takes a vigilant, organized approach to three core areas of stroke patient care at home: medication management, specialized nutrition, and watching for complications.
Getting these right is so much more than just following a checklist. It's about creating systems that genuinely reduce risk and give the body what it needs to heal. Each piece is connected—the right medications help stabilize their health, good nutrition fuels recovery, and your sharp eye catches small problems before they become big ones.
This detailed, personal management is a huge reason why home-based care is often so effective. A landmark 20-year UK study showed that survival was significantly better for individuals who went home after a stroke. What's more, medication adherence for preventing a second stroke jumped to 56.3% at home, compared to just 38.1% in care facilities. It just goes to show how a dedicated home environment makes all the difference.
Creating a Flawless Medication Routine
It's common for a stroke survivor to come home from the hospital with a complex list of new prescriptions, from blood thinners to blood pressure meds. Without a solid system, managing that list is overwhelming and, frankly, dangerous. The first step is to create absolute clarity.
Start with a master list of all medications. Write down the name, dosage, time of day, and what each pill is for. A weekly pill organizer is a non-negotiable tool here. It lets you set up everything for the week at once, which drastically cuts down on missed or double doses. Back that up with daily alarms on a phone or clock.
It's also crucial to know the potential side effects so you're not caught off guard.
- Dizziness or Lightheadedness: This is common with blood pressure medication and can increase the risk of a fall.
- Bruising Easily: Often happens with blood thinners. Be sure to report any large or unusual bruising to their doctor right away.
- Stomach Upset: Some medications are just better with food to avoid irritation.
When you know what to expect, you can tell the difference between a normal side effect and a sign of a bigger problem. For families juggling a particularly complex regimen, professional support in senior medication management can be an invaluable safety net.
The goal is to make the medication process automatic and error-proof. Consistency is the most powerful tool you have for preventing another stroke and managing related health conditions.
Addressing Nutrition and Swallowing Challenges
Nutrition after a stroke is about much more than just healthy eating; it's about adapting to new physical challenges. Many survivors develop dysphagia (difficulty swallowing), which puts them at a high risk for choking and aspiration pneumonia.
A speech-language pathologist will likely recommend a specific food texture to keep them safe. This might mean changing their diet to include things like:
- Pureed Foods: Smooth, pudding-like consistency with absolutely no lumps.
- Minced & Moist Foods: Soft, tiny lumps that are easy to mash with a fork.
- Soft & Bite-Sized Foods: Tender foods that still need some chewing but are easy to manage.
Staying hydrated is just as important, but it can be a real challenge with dysphagia. You may need to thicken liquids to a nectar, honey, or pudding-like consistency. This slows them down, allowing for a safer swallow. Always make sure your loved one is sitting fully upright during meals and for at least 30 minutes afterward.
Staying Vigilant for Potential Complications
As a caregiver, you are the first line of defense in spotting complications. Knowing the warning signs means you can act fast and get medical help when it's needed most.
One of the most critical things to monitor for is a second stroke. Always remember the F.A.S.T. acronym:
- Face Drooping
- Arm Weakness
- Speech Difficulty
- Time to call emergency services
Beyond another stroke, keep an eye out for other issues. Deep vein thrombosis (DVT), a blood clot in the leg, can show up as swelling, pain, or redness in one leg. Also watch for signs of infection, like a fever or changes in breathing, especially if your loved one has mobility issues. This is where a trained in-home caregiver can be a tremendous asset, as they're skilled in monitoring vitals and picking up on subtle changes that need a doctor's attention.
Setting Up a Safe and Supportive Home
When your loved one comes home after a stroke, your living space needs to do more than just be comfortable—it has to become an active partner in their recovery. Excellent stroke patient care at home means transforming the environment into one that’s not just safe, but truly rehabilitative. The real goal here is to design a space that cuts down on risks while creating every possible opportunity for them to rebuild their independence and strength.
This is all about looking at your home with fresh eyes. You'll need to spot potential hazards and make smart, practical changes. It goes way beyond just preventing falls; you're building a home that actively supports the hard work of rehabilitation, day in and day out.
A Room-by-Room Safety Check
The best way to start is to walk through your home and try to see it through their eyes. Imagine navigating the space with limited mobility, shaky balance, or weakness on one side of your body. This simple exercise will make the most urgent modifications immediately obvious.
The Bathroom: Your Top Priority
This room is almost always the most hazardous spot in the house for someone recovering from a stroke.
- Install grab bars inside the shower and right next to the toilet. These are absolutely non-negotiable and provide crucial support.
- Get a shower chair or transfer bench. This makes bathing much safer and far less exhausting.
- Put down non-slip mats both inside and outside the tub or shower. Wet floors are a recipe for disaster.
- A raised toilet seat can make a world of difference, reducing the strain on weak muscles when sitting or standing.
Living Areas and Hallways: Clear the Way
For these common areas, your main focus should be on creating clear, wide, and unobstructed pathways.
- Get rid of all throw rugs and runners. They are one of the most common tripping hazards, period.
- Tuck away or secure any loose electrical cords along the baseboards so they’re not a danger.
- Make sure there is plenty of lighting everywhere, especially in hallways and on staircases. Nightlights are a huge help for getting around after dark.
- Rearrange the furniture to leave wide-open paths, giving enough space for a walker or even a wheelchair to pass through easily.
A safe home does so much more than just prevent accidents—it builds confidence. When a stroke survivor feels secure moving around their own space, they become more willing to practice their mobility and take part in daily life.
It's also important to think about the overall health of the indoor environment. Keeping the air free from allergens and irritants is vital. For example, knowing the basics of preventing mold in basements can dramatically improve air quality, which is especially important for someone whose system is already under stress.
Designing a Home That Encourages Recovery
A truly supportive home environment goes beyond just basic safety tweaks. You want to set things up to encourage movement and make therapy exercises feel like a natural part of the day.
Think about how you can organize rooms to foster independence. In the kitchen, for example, try moving frequently used items—plates, glasses, favorite snacks—to lower shelves that are easy to reach. It might seem like a small change, but it empowers your loved one to do things for themselves, which is a huge step toward regaining their autonomy.
Create a Dedicated Rehab Space
You don't need anything fancy. Just set up a designated "rehab corner" in a main living area. A comfortable chair, a small table, and a basket with their therapy tools (like resistance bands, therapy putty, or small weights) is all it takes to create a dedicated spot for their daily exercises.
Having everything in one place serves as a great visual reminder and makes it much easier to stick to the therapy schedule. This is where an in-home caregiver can be incredibly helpful, maintaining this safe space while offering encouragement during those daily sessions. It’s this kind of structure that helps turn repetitive exercises into consistent, progress-building habits.
Sustaining Yourself on The Caregiver's Path
The journey of stroke patient care at home is an endurance event, not a sprint. Your focus is naturally on your loved one’s recovery, but your own well-being is the foundation that supports everything else. If you collapse, the whole system collapses.
This is where we need to have an honest conversation about the immense physical and emotional weight of caregiving. The constant vigilance, the demands of transfers and personal care, and the emotional toll of seeing someone you love struggle can lead to profound exhaustion. Recognizing this isn't a sign of weakness—it's the first step toward building resilience.

The reality is, informal caregivers shoulder an incredible burden, often with very little outside help. One study highlighted that caregivers for stroke survivors are often middle-aged and navigating this complex new role with minimal formal support—in fact, only 12% had access to government home care services. This really underscores how vital it is to build your own support network before you’re running on empty.
Recognizing and Preventing Caregiver Burnout
Burnout isn’t just about feeling tired. It’s a state of emotional, physical, and mental exhaustion that creeps in after prolonged stress, slowly draining your energy and optimism. It's crucial to stay aware and recognize signs of emotional burnout before it takes over.
Keep an eye out for these red flags:
- Persistent Fatigue: A deep-seated exhaustion that a full night's sleep just doesn't seem to touch.
- Increased Irritability: Finding yourself short-tempered or resentful toward others, even your loved one.
- Social Withdrawal: Losing interest in hobbies and pulling away from friends and social plans you used to enjoy.
- Changes in Health: Noticing more frequent headaches, stomach issues, or just generally getting sick more often.
Preventing burnout requires a conscious, daily effort to protect your own energy. It means giving yourself permission to step back, recharge, and ask for help without feeling guilty.
The Lifeline of Respite Care and Support Systems
You simply cannot pour from an empty cup. This is where respite care becomes an absolute necessity, not a luxury. Think of it as a planned, guilt-free break for you, the primary caregiver. It can be for a few hours a week to run errands or a few days to truly rest and recharge.
During this time, a professional caregiver from an agency like NJ Caregiving can step in, ensuring your loved one receives seamless, expert care. This gives you invaluable peace of mind, allowing you to actually disconnect knowing they are safe and in good hands.
Building a solid support system is equally important. This means having clear, honest conversations with other family members about sharing the load. A shared calendar for appointments or regular check-in calls can help divide tasks and provide emotional backup for one another. Don't overlook support groups, either online or in person—they can be a fantastic way to connect with others who truly get what you're going through.
Below is a simple plan to help you stay ahead of burnout by identifying common challenges and putting preventative strategies in place.
Caregiver Burnout Prevention Plan
| Challenge | Preventative Strategy | How Professional Respite Care Helps |
|---|---|---|
| Physical Exhaustion | Schedule regular, non-negotiable breaks each day and week. Prioritize your own sleep. | Provides dedicated time off to rest and recover, knowing your loved one is safe. |
| Emotional Drain | Talk to a trusted friend, join a support group, or consider professional counseling to process your feelings. | Offers an emotional break from the constant demands and worry, reducing stress. |
| Social Isolation | Make a point to schedule coffee with a friend, attend a class, or continue a hobby you enjoy. | Frees up time in your schedule to maintain social connections and personal interests. |
| Overwhelm from Tasks | Delegate specific tasks (like grocery shopping or paying bills) to other family members or friends. | A professional caregiver can handle personal care, light housekeeping, and meal prep, lightening your load. |
Remember, taking care of yourself isn't selfish—it's a critical component of providing the best possible care for your loved one. By actively managing your own well-being, you ensure you have the strength and resilience needed for the long haul.
Common Questions About Home Stroke Care
Bringing a loved one home after a stroke is a huge step, and it naturally comes with a flood of questions. As families find their footing in this new reality, practical concerns quickly bubble to the surface. Getting clear answers builds confidence and helps make the transition from hospital to home a much smoother, safer experience for everyone.
Let’s walk through some of the most pressing questions we hear from families. Our goal is to demystify the essential parts of home care, from making the house safe to figuring out how to pay for the support you need.
Is My Home Safe Enough for a Stroke Patient?
This is the absolute first thing to tackle. Making your home safe starts with a critical walk-through, looking at everything through the lens of fall prevention. You’d be surprised how a few simple changes can make a world of difference for your loved one's safety and confidence.
The bathroom is priority number one.
- Install sturdy grab bars next to the toilet and inside the shower. These aren't just nice to have; they are essential for stability.
- Use a shower chair or transfer bench. This makes bathing much safer and less exhausting for both of you.
- Lay down non-slip mats in the tub and on the floor. Wet surfaces are a recipe for disaster, and this is an easy fix.
Once the bathroom is handled, scan the rest of your living space. Get rid of all throw rugs—they are a notorious tripping hazard. Make sure electrical cords are tucked away along walls and that there are wide, clear pathways in every room. Good lighting is also key, especially at night, so add nightlights in hallways and bathrooms. A professional home care agency can even do a full safety assessment during an initial visit, pointing out things you might have missed.
What Is the Difference Between Home Health and In-Home Caregiving?
This is a big point of confusion for many families, but the distinction is really important. The easiest way to think about it is clinical medical care versus daily life support.
Home health care is skilled medical care that a doctor prescribes, usually for a set period after someone leaves the hospital. This is when you'll see a licensed professional—like a nurse, physical therapist, or occupational therapist—coming to the home. They handle specific medical tasks like wound care, giving injections, or leading formal therapy sessions.
In-home caregiving, on the other hand, is non-medical personal support that focuses on the Activities of Daily Living (ADLs). A professional caregiver is there to help with things like bathing, getting dressed, preparing meals, moving around the house safely, providing medication reminders, and offering companionship.
While home health tackles specific medical recovery goals, in-home care provides the consistent, day-to-day support that ensures a stroke survivor can live at home with safety, comfort, and dignity. The two services often work together, creating a complete circle of care.
How Can We Pay for In-Home Care?
The cost of care is, understandably, a major concern. The good news is that there are several ways to fund the support your family needs. Knowing your options is the first step in creating a plan that works long-term.
Many families pay for services directly, which is known as private pay. It’s also worth digging out any long-term care insurance policies your loved one might have, as they often cover in-home caregiving. You’ll want to review the policy closely to understand the benefits and any coverage limits.
Government programs are another crucial resource. In New Jersey, for example, Medicaid-eligible individuals can get coverage for home-based services through programs like Managed Long-Term Services and Supports (MLTSS). If your loved one is a veteran, the Department of Veterans Affairs (VA) may also offer assistance.
Trying to navigate these programs alone can feel overwhelming, but an experienced home care agency can be an invaluable guide. They often help families figure out what they’re eligible for and walk them through the applications, taking a huge administrative burden off your shoulders so you can focus on your loved one.
At NJ Caregiving, we understand the complexities of arranging stroke patient care at home. Our team is here to guide you through every step, from creating a safe environment to navigating payment options, ensuring your loved one receives compassionate and expert support. Learn how we can help your family in Princeton and Mercer County.


