Medication is a cornerstone of modern healthcare, but its management is fraught with risk. For seniors and their caregivers, navigating complex medication regimens can be daunting, and the potential for error is a serious concern. A single mistake, such as a wrong dose, an overlooked interaction, or a missed medication, can have significant health consequences. This guide is dedicated to outlining powerful, evidence-based medication error prevention strategies that enhance safety and provide peace of mind.
We will explore seven critical strategies, moving from cutting-edge technologies to fundamental process improvements that are transforming patient care. This article provides actionable insights for anyone involved in managing medications, whether you are a family member providing care at home, a senior self-managing your health, or a healthcare professional coordinating treatment plans. Understanding these methods is the first step toward creating a safer environment.
The focus here is on practical implementation. You will learn about specific tools and protocols that can be adopted to minimize risk and improve health outcomes. By implementing these detailed strategies, caregivers and patients can work together more effectively, ensuring that medications serve their intended purpose: to heal without causing harm. We will cover the following key areas:
- Computerized Provider Order Entry (CPOE) Systems
- Barcode Medication Administration (BCMA)
- Clinical Pharmacist Integration
- Medication Reconciliation Protocols
- Smart Infusion Pumps with Drug Libraries
- Standardized Medication Labeling and Storage
- Automated Dispensing Systems
1. Computerized Provider Order Entry (CPOE) Systems
One of the most impactful medication error prevention strategies implemented in modern healthcare is the adoption of Computerized Provider Order Entry (CPOE) systems. These platforms replace traditional, error-prone handwritten prescriptions with a direct, digital process. Healthcare providers enter medication orders, lab requests, and other instructions into a computer, which then transmits them directly to the pharmacy, laboratory, or other relevant departments.
The primary strength of CPOE lies in its ability to eliminate illegible handwriting, a notorious source of dangerous medication errors. By creating a standardized, digital record from the moment of prescription, these systems drastically reduce the risk of transcription mistakes. This foundational change is why CPOE is a cornerstone of patient safety initiatives championed by organizations like The Leapfrog Group and implemented by leading health systems such as Epic and Cerner.
How CPOE Enhances Medication Safety
CPOE systems do more than just digitize prescriptions; they are powerful tools for clinical decision support. As a provider enters an order, the system cross-references it with the patient's electronic health record (EHR) in real-time. This integration provides an immediate safety net, flagging potential issues before they can cause harm.
Key safety alerts include:
- Drug-Drug Interactions: Warns if a newly prescribed medication will negatively interact with a patient's current medications.
- Allergy Alerts: Flags any known allergies to the prescribed drug or its components.
- Dosing Errors: Verifies that the dosage is appropriate for the patient's age, weight, and kidney function, preventing under- or overdosing.
- Duplicate Therapy Alerts: Notifies the provider if the same or a similar medication is already prescribed.
"The transition from paper to CPOE is not just a technological upgrade; it's a fundamental shift in the culture of safety. It introduces multiple, automated checkpoints that catch human errors before they reach the patient." – Dr. David Bates, a pioneer in CPOE research.
The following infographic highlights key data points demonstrating the effectiveness of these systems in reducing medication errors.
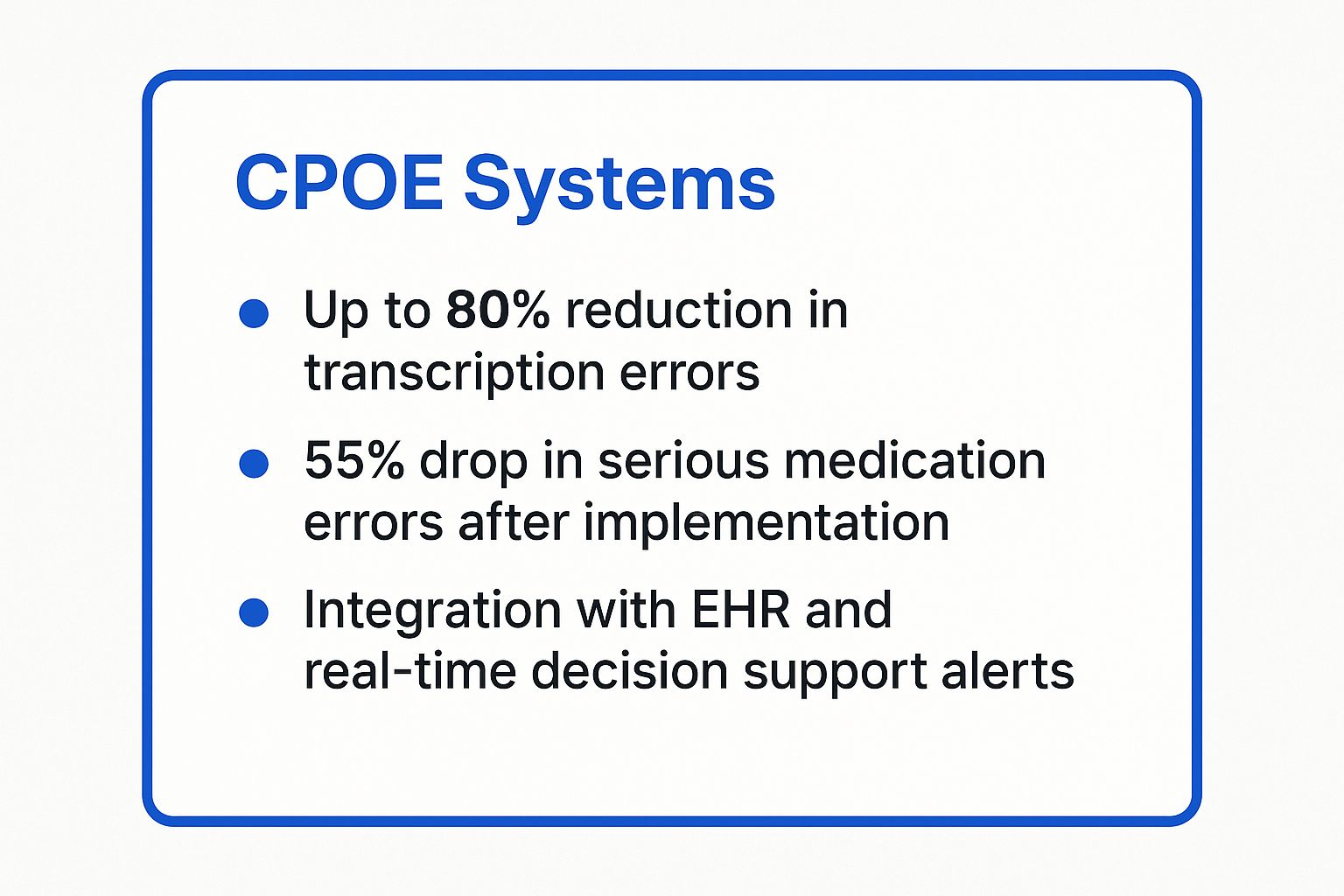
As the data shows, the impact is significant, with some hospitals seeing serious medication errors fall by more than half after successful implementation. This success is often replicated across different healthcare settings. For example, studies at Brigham and Women's Hospital and Veterans Affairs medical centers have shown dramatic reductions in adverse drug events after adopting CPOE. For family caregivers and patients, this technology provides peace of mind, knowing that a powerful digital safety net is in place.
2. Barcode Medication Administration (BCMA)
A crucial technology-driven approach to enhancing medication error prevention strategies is the implementation of Barcode Medication Administration (BCMA) systems. This method acts as a real-time safety check at the patient's bedside by electronically verifying the "Five Rights" of medication administration: the right patient, right drug, right dose, right route, and right time. Before giving a medication, a nurse or caregiver scans the barcode on the patient's wristband and then the barcode on the medication itself.
The system's core function is to create an immediate, automated verification loop that closes the circle of medication safety. It cross-references the scanned information with the patient's electronic medication administration record (eMAR), instantly alerting the user to any discrepancies. This digital safeguard, strongly advocated for by organizations like the Institute for Safe Medication Practices (ISMP) and The Joint Commission, transforms the point of administration from a high-risk manual task into a verified, technology-assisted process.

How BCMA Enhances Medication Safety
BCMA systems directly prevent errors that can occur during the final and most vulnerable step of the medication process: administration. By requiring a scan of both the patient and the medication, it confirms identity and prescription details with near-perfect accuracy, something a manual check can never guarantee. This system is designed to catch "wrong patient," "wrong drug," and "wrong dose" errors before they happen.
Key safety functions include:
- Patient Verification: Confirms that the medication is being given to the correct individual, preventing mix-ups in multi-patient settings.
- Medication Matching: Validates that the drug, dose, and route match the physician's order in the eMAR.
- Timing Alerts: Flags if a medication is being administered too early, too late, or has already been given.
- Documentation Automation: Automatically records the administration time, dose, and person who gave the medication, improving accuracy and saving time.
"BCMA is the last line of defense. It's the final, critical check that ensures the right medication gets to the right patient. Its implementation has been one of the most significant advances in preventing bedside medication errors." – A leading patient safety advocate from the Institute for Safe Medication Practices (ISMP).
The results of BCMA implementation are well-documented and compelling. For example, the Mayo Clinic reported a 47% reduction in medication errors across all its hospital units after adopting the system. Similarly, the University of Maryland Medical Center saw wrong-patient errors decrease by a remarkable 63%. For family caregivers managing complex medication schedules at home or in facilities, the presence of BCMA provides a powerful assurance that a reliable safety protocol is being followed every single time a medication is administered.
3. Clinical Pharmacist Integration
Another of the most effective medication error prevention strategies is the integration of clinical pharmacists directly into patient care teams. This approach moves the pharmacist from a traditional dispensing role to an active, collaborative position alongside doctors and nurses. Clinical pharmacists participate in patient rounds, conduct in-depth medication reconciliations, and provide specialized consultations, acting as dedicated medication safety experts at the point of care.
The core value of this strategy is the pharmacist's specialized expertise in pharmacotherapy. By embedding this knowledge within the clinical team, healthcare providers gain a real-time resource for complex medication decisions. This proactive involvement is a central tenet of patient safety advocated for by leading organizations like the American Society of Health-System Pharmacists (ASHP) and the American College of Clinical Pharmacy (ACCP), which champion the pharmacist's role in optimizing medication use and preventing harm.
How Clinical Pharmacists Enhance Medication Safety
Integrating a pharmacist into the care team creates a powerful, human-centered safety check that complements technological solutions. Their focused training allows them to identify subtle yet critical medication issues that automated systems might miss. They serve as a crucial second set of expert eyes, evaluating the appropriateness and safety of every medication order within the full context of a patient's condition.
Key safety functions include:
- Comprehensive Medication Reviews: Analyzing a patient's entire medication list, including over-the-counter drugs and supplements, to identify risks and optimize therapy.
- Dose Adjustment: Recommending precise dosage adjustments based on a patient's lab results, particularly kidney and liver function, to prevent toxicity.
- Therapeutic Monitoring: Ensuring medications are achieving the desired effect without causing adverse reactions, and suggesting alternatives when necessary.
- Patient Education: Directly counseling patients and family caregivers on how to take medications correctly, what side effects to watch for, and the importance of adherence.
"Placing a pharmacist on the ward is not an added cost; it's a high-yield investment in patient safety. They are uniquely trained to see the entire medication picture, catching potential errors and optimizing therapy in a way no other professional can." – Dr. Heather Draper, University of Birmingham.
The following data from pioneering health systems demonstrates the profound impact of this integrated model on patient safety.
As the data illustrates, the results are consistently impressive. For instance, Johns Hopkins Hospital saw a 50% reduction in medication errors after integrating pharmacists into its teams, while the University of Colorado Hospital reported a 66% decrease in adverse drug events thanks to pharmacist-led interventions. For family caregivers, having access to a clinical pharmacist provides an invaluable resource for asking detailed medication questions and ensuring their loved one's regimen is both safe and effective.
4. Medication Reconciliation Protocols
A crucial strategy for preventing medication errors involves implementing rigorous medication reconciliation protocols. This is a systematic process of creating the most accurate list possible of all medications a patient is taking. The list includes drug name, dosage, frequency, and route and is then compared against new medication orders at every transition of care, such as upon hospital admission, when moving between units, or at discharge.

The primary goal of this medication error prevention strategy is to identify and resolve discrepancies like omissions, duplications, dosing errors, or unwanted interactions. By ensuring a seamless and accurate flow of medication information, these protocols prevent the harmful gaps and overlaps that often occur when a patient moves through different healthcare settings. This approach is strongly endorsed by leading safety organizations, including The Joint Commission and the World Health Organization (WHO), as a foundational patient safety practice.
How Medication Reconciliation Enhances Medication Safety
Medication reconciliation serves as a critical safety net, directly addressing the communication failures that lead to adverse drug events. The process formalizes the comparison of a patient’s home medication list with what is newly ordered, creating a single, verified source of truth. This proactive verification is essential for ensuring continuity of care and preventing preventable harm.
Key safety benefits include:
- Preventing Omissions: Ensures that essential long-term medications, like those for blood pressure or diabetes, are not accidentally stopped during a hospital stay.
- Eliminating Duplications: Identifies instances where a generic drug might be prescribed alongside a brand-name version of the same medication, preventing overdose.
- Correcting Dosing Errors: Catches discrepancies between the patient's reported home dosage and what is ordered in a new care setting.
- Identifying Unintended Discontinuations: Verifies that any medications stopped were intentionally discontinued by a provider and not simply forgotten during a care transition.
"Medication reconciliation is not just a task to be checked off; it is a critical thinking process. It requires a partnership between clinicians, patients, and families to piece together the puzzle of a patient's full medication regimen." – Institute for Healthcare Improvement (IHI)
The impact of structured reconciliation is well-documented. For instance, Massachusetts General Hospital saw a 42% reduction in medication errors after implementing a standardized reconciliation process. Similarly, the Cleveland Clinic's comprehensive program led to an 18% decrease in hospital readmissions. For family caregivers, actively participating in this process by providing an up-to-date medication list can be one of the most effective ways to advocate for their loved one’s safety.
5. Smart Infusion Pumps with Drug Libraries
A critical strategy for preventing medication errors in settings where intravenous (IV) drugs are administered is the use of smart infusion pumps. Unlike traditional pumps, these advanced devices are equipped with Dose Error Reduction Software (DERS) and a built-in drug library. This library contains pre-programmed medication parameters, including safe dose limits, concentration ranges, and administration guidelines specific to the institution.
The core function of a smart pump is to act as an active safety net during IV medication setup. When a nurse or clinician programs an infusion, the pump cross-references the entered data against the established safety limits in its drug library. If the programmed rate, dose, or concentration falls outside the safe range, the pump issues an alert, prompting the clinician to double-check the order before the infusion begins. This intervention is a powerful tool in preventing potentially fatal overdoses or ineffective under-doses.
How Smart Pumps Enhance Medication Safety
Smart infusion pumps go beyond simple rate control; they are intelligent gatekeepers for high-risk medications. By standardizing IV administration practices and providing real-time decision support at the point of care, they significantly reduce the chance of human error. This technology is championed by leading safety organizations like the Institute for Safe Medication Practices (ISMP) and integrated into devices from manufacturers such as BD (Becton Dickinson) and ICU Medical.
Key safety features include:
- Dose Error Reduction: Alerts clinicians if a programmed dose is too high (hard limit) or too low (soft limit), preventing keypad entry mistakes.
- Customized Drug Libraries: Allows hospitals to create profiles for different care areas, such as pediatrics or intensive care, with specific drug parameters for each patient population.
- Clinical Advisories: Provides on-screen guidance and reminders for specific medications, such as the need for a secondary check or specific patient monitoring.
- Data Analytics: Gathers data on alerts, overrides, and compliance, which can be analyzed to identify trends and drive continuous quality improvement initiatives.
"Smart pumps are not just a piece of equipment; they are an active partner in patient safety. By providing an intelligent, automated double-check, they empower clinicians to catch and correct potential errors before they can ever cause harm." – Institute for Safe Medication Practices (ISMP) recommendation.
The real-world impact of this technology is well-documented. For instance, Texas Children's Hospital successfully reduced high-risk medication errors by 73% after implementing smart pumps. Similarly, Scripps Health reported preventing over 1,000 potential medication errors annually with the help of its smart pump system. These examples underscore why smart pumps are a fundamental component of modern medication error prevention strategies in hospitals and other clinical settings. For families with loved ones receiving IV therapy, knowing a smart pump is in use provides an added layer of assurance.
6. Standardized Medication Labeling and Storage
A surprisingly common yet dangerous source of medication errors stems from simple visual confusion. Standardized medication labeling and storage is a systematic strategy designed to minimize these risks by making it easier to distinguish between different drugs, especially those with similar names or packaging. This approach involves creating and enforcing consistent rules for how medications are labeled, packaged, and physically organized, thereby reducing the chance of a caregiver or patient grabbing the wrong bottle.
The core principle of this strategy is to create clear visual cues that override potential confusion. This is particularly crucial for "look-alike, sound-alike" (LASA) medications. By implementing standards for label formats, color-coding, and storage systems, healthcare providers and at-home caregivers can build a safer medication environment. This is one of the key medication error prevention strategies endorsed by leading patient safety organizations like the Institute for Safe Medication Practices (ISMP) and The Joint Commission.
How Standardization Enhances Medication Safety
Standardization directly addresses human factors that lead to errors, such as confirmation bias and slips in attention. By making medication labels and storage locations predictable and visually distinct, it adds a crucial layer of verification that is easy to follow. This system-level approach provides a powerful defense against mix-ups.
Key safety components include:
- Tall Man Lettering: This technique, promoted by the FDA, uses a mix of lower- and upper-case letters to emphasize the differences between similar drug names (e.g., hydrOXYzine and hydrALAzine).
- Consistent Color-Coding: Assigning specific colors to certain classes of drugs or high-alert medications can provide an immediate visual warning.
- Clear Label Formats: Standardizing where information like the drug name, strength, and expiration date appears on a label makes it faster and easier to verify.
- Segregated Storage: Physically separating medications with similar names or packaging in different bins, shelves, or drawers in a medicine cabinet or pharmacy.
"A well-organized medication cabinet isn't just about being tidy; it's a critical safety tool. When labels are clear and similar drugs are separated, you are actively designing a system that makes it hard to make a mistake." – Institute for Safe Medication Practices (ISMP) publication.
The impact of these methods is well-documented. For instance, Kaiser Permanente successfully reduced medication selection errors by 75% after implementing a standardized labeling program. Similarly, a study at the Children's Hospital of Philadelphia found that using tall man lettering helped decrease errors involving specific LASA drug pairs by 45%. For family caregivers managing multiple prescriptions for a loved one, adopting these principles at home can significantly reduce the risk of a dangerous mix-up.
7. Automated Dispensing Systems
Another powerful strategy for preventing medication errors involves the use of Automated Dispensing Systems (ADS), often called automated dispensing cabinets or ADCs. These are secure, computer-controlled storage units that dispense medications at the point of care, such as on a hospital floor or in a long-term care facility. They replace traditional, open-access medication rooms with a system that requires user authentication, tracks every dose, and provides a robust audit trail.
The core benefit of ADS is its ability to ensure the right medication gets to the right patient at the right time through a controlled, documented process. By securing the medication supply and requiring verification before access, these systems drastically reduce the risk of human error, such as grabbing the wrong drug from a shelf. Leading organizations like the American Society of Health-System Pharmacists (ASHP) and companies such as Omnicell and BD (Becton, Dickinson) have championed their use as a key safety measure.
How ADS Enhances Medication Safety
Automated Dispensing Systems provide a critical layer of security and accuracy directly where medications are administered. They function as decentralized, intelligent pharmacies, integrating directly with the pharmacy information system and the patient's electronic health record (EHR) to create a closed-loop medication process. This integration prevents errors before they happen.
Key safety features include:
- Controlled Access: Requires a unique user login and often a second verification (like a fingerprint scan), creating a clear record of who accessed medication and when.
- Guided Dispensing: The system guides the user directly to the correct medication by illuminating the specific drawer or bin, preventing look-alike/sound-alike drug mix-ups.
- Real-Time Inventory: Tracks medication stock levels automatically, reducing the risk of a needed dose being unavailable and preventing stock-outs or overstocking.
- Enhanced Security: Significantly reduces medication diversion and theft, ensuring that controlled substances are accounted for with precision.
"Automated dispensing systems are the gatekeepers of medication safety at the point of care. They don't just store drugs; they actively participate in the verification process, creating a reliable checkpoint between the pharmacy's order and the patient's bedside." – Institute for Safe Medication Practices (ISMP) Report.
The impact of ADS is well-documented. For instance, Mercy Health System saw an 85% reduction in medication variances after implementation. Similarly, Stanford Health Care improved medication availability while cutting errors by 35%. For family caregivers in a facility setting, knowing that such a system is in place provides reassurance that an advanced, technological safeguard is protecting their loved one from administration errors.
Medication Error Prevention Strategies Comparison
| Item | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Computerized Provider Order Entry (CPOE) Systems | High – $2-10M; extensive training | High – IT infrastructure + staff time | Up to 80% reduction in transcription errors; 40-55% med error reduction | Hospitals needing standardized, EHR-integrated ordering | Real-time alerts; audit trails; error reduction |
| Barcode Medication Administration (BCMA) | Moderate – $100K-500K; workflow changes | Moderate – barcode hardware + training | 25-50% med admin error reduction; up to 65% reduction in wrong-patient errors | Point-of-care med verification in nursing units | Improved patient ID; real-time error alerts |
| Clinical Pharmacist Integration | Moderate – hiring + workflow redesign | High – additional pharmacist salaries | 50-78% reduction in adverse drug events; 10-15% fewer readmissions | Multidisciplinary teams in hospitals | Medication expertise; cost savings; adherence |
| Medication Reconciliation Protocols | Moderate – staff time intensive | Moderate – dedicated staff & training | 70-95% medication discrepancy reduction; fewer adverse events | Care transitions (admission, transfer, discharge) | Prevents omissions/duplications; improves communication |
| Smart Infusion Pumps with Drug Libraries | Moderate-High – $5K-15K per pump; updates | High – devices + maintenance + training | 50-85% reduction in IV med errors; near 99% safety compliance | IV medication administration requiring dose safety | Real-time dose checks; customizable libraries |
| Standardized Medication Labeling and Storage | Moderate – relabeling + physical changes | Moderate – materials + training | 60-80% reduction in look-alike/sound-alike errors | Pharmacies and medication preparation areas | Visual differentiation; reduces selection errors |
| Automated Dispensing Systems | High – $40K-100K/unit; technical support | High – equipment + ongoing maintenance | 25-40% medication error reduction; improved security and audit trails | Secure medication access at point of care | Inventory control; diversion reduction; audit trails |
Fostering a Culture of Safety in Medication Management
Preventing medication errors is not a task accomplished with a single tool or a one-time fix. Instead, it requires building a robust, multi-layered system of safety where each component reinforces the others. The seven medication error prevention strategies detailed throughout this article represent the pillars of modern patient safety, creating a formidable defense against potential harm. From the technological precision of Computerized Provider Order Entry (CPOE) and Barcode Medication Administration (BCMA) to the critical human oversight provided by Clinical Pharmacist Integration and Medication Reconciliation, each strategy plays a vital role.
These approaches are not isolated solutions but interconnected parts of a cohesive safety ecosystem. Smart infusion pumps prevent dosage miscalculations, while standardized labeling and automated dispensing systems reduce the risk of human error in handling and distribution. Together, they form a safety net, catching potential mistakes before they can reach the patient. Embracing these advanced practices is a commitment to excellence in care.
The Power of a Multi-Pronged Approach
The true strength of these strategies lies in their combined application. A CPOE system can eliminate handwriting errors, but its effectiveness is magnified when paired with a clinical pharmacist who reviews the order for appropriateness. Similarly, a BCMA system ensures the right patient gets the right drug, but its success depends on the accurate information entered during medication reconciliation.
This synergy highlights a fundamental truth: technology empowers, but it does not replace, human diligence. A proactive and vigilant approach from every member of the care team, including patients and their families, is the glue that holds these systems together. This integrated framework is the gold standard for achieving comprehensive medication safety.
Key Takeaway: The most effective medication error prevention strategies are not implemented in isolation. True safety emerges from the integration of technology, standardized processes, and dedicated professional oversight, creating multiple checkpoints to intercept errors.
Actionable Next Steps for Caregivers and Families
Building a culture of safety begins with proactive steps. For family caregivers and seniors managing complex medication schedules, the principles behind these clinical strategies can be adapted for home use. Your immediate goal should be to create your own system of checks and balances.
Your Action Plan:
- Create a Master Medication List: Immediately compile and maintain an up-to-date list of all medications, including prescriptions, over-the-counter drugs, and supplements. Use a digital app or a clear, written document.
- Become the "Reconciliation Expert": Bring your master list to every single doctor's appointment, hospital visit, and pharmacy pickup. Actively compare the list with what the provider has on record to catch discrepancies.
- Leverage Simple Technology: Use pill organizers with daily compartments, set smartphone alarms for each dose, and explore apps that provide medication reminders and track adherence. This mirrors the function of automated dispensing on a personal scale.
- Advocate and Communicate: Never hesitate to ask clarifying questions. If a new pill looks different or instructions are unclear, verify with the pharmacist or doctor before administering it. Empower your loved one to speak up if something feels wrong.
By implementing these actionable steps, you are translating proven medication error prevention strategies from the clinical setting into your home. This disciplined approach is invaluable, transforming routine medication management into a structured, safety-focused process. It ensures clarity, promotes consistency, and significantly reduces the risk of dangerous mistakes, ultimately protecting the health and well-being of those you care for. This dedication is the cornerstone of providing safe, effective, and compassionate care.
Navigating complex medication schedules requires expertise and unwavering attention to detail. If you are seeking professional support to implement these safety strategies at home, the compassionate caregivers at NJ Caregiving are trained in medication management protocols to ensure your loved one's safety and well-being. Visit NJ Caregiving to learn how our dedicated team can provide the peace of mind you deserve.



