When you’re dealing with a long-term health issue, healthcare can feel like a series of fires to put out—a sudden flare-up, a new symptom, an unexpected trip to the doctor. But what if it was less about reacting to crises and more about preventing them in the first place?
That’s the core idea behind chronic disease management. It’s a completely different way of thinking about long-term health. Instead of just treating symptoms as they pop up, it’s a proactive, organized partnership between your loved one, your family, and their healthcare team. The goal is simple but powerful: improve daily life, slow the disease down, and keep your loved one living as comfortably and independently as possible.
A Proactive Partnership for Long-Term Wellbeing
Think of it like tending a garden versus calling the fire department. You don’t wait for the plants to wither before you water them; you provide consistent care—water, sunlight, weeding—to keep them healthy and thriving. Chronic disease management applies that same steady, forward-thinking approach to a person's health.
It brings everyone to the table: the patient, their family, doctors, specialists, and caregivers. Together, they create a sustainable plan that looks at the big picture, preventing breakdowns before they happen.
The Growing Need for Management
This isn't just a niche concept; it's becoming essential. The numbers are hard to ignore. In 2023, an incredible 76.4% of adults in the United States were living with at least one chronic condition, and more than half were juggling two or more.
For families in communities like Princeton, NJ, this isn't just a statistic. It's the daily reality of helping a parent manage diabetes, heart disease, or Parkinson's. The need for a structured, supportive approach is greater than ever. You can dig deeper into these trends in this research on chronic condition statistics.
A successful management plan does more than just address medical needs. It creates a safety net that empowers seniors, preserves their independence, and provides invaluable peace of mind for their families.
From Concept to Daily Reality
So, what does this look like day-to-day? For seniors in New Jersey who want to age in place, it means turning a doctor's complex instructions into simple, manageable routines. It's the practical, on-the-ground work of making sure medications are taken correctly, diet is followed, and small changes are noticed before they become big problems.
This is where partners like NJ Caregiving come in, helping to translate the medical plan into real-world support. This hands-on coordination is a key part of what makes it work, similar to the philosophy behind geriatric care management. To see how these concepts connect, take a look at our guide on what is geriatric care management.
Ultimately, chronic disease management is about providing continuous, all-encompassing support. It's what allows someone to not just live with their condition, but to truly thrive despite it.
The Core Components of an Effective Care Plan
Chronic disease management sounds like a big, complicated idea, but when you break it down, it’s really about a practical, life-changing strategy built on a few essential parts. Think of it like building a house: you need a solid foundation, strong walls, and a protective roof, all working together. An effective care plan is built the same way, on five crucial pillars that support one another.
These components turn care from a series of disconnected doctor’s visits into a cohesive, day-in-day-out system that actually improves your loved one's well-being. Each element has a unique job, from creating a personalized roadmap to making sure everyone involved is on the same team.
This diagram really shows how collaborative the whole process is, with the patient right at the center, supported by family, caregivers, and medical providers.
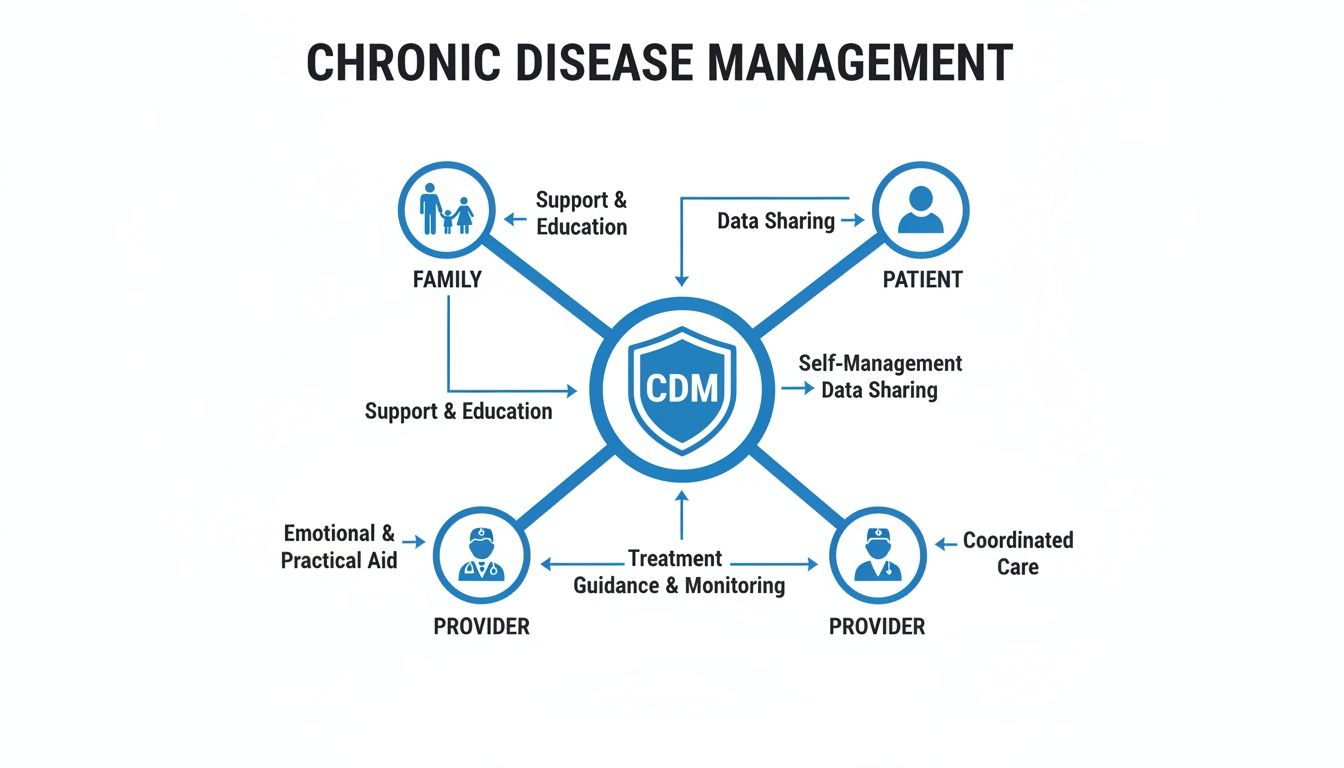
It’s a great visual reminder that success isn't just about medicine—it’s about the strong, interconnected support system you build around someone.
Personalized Care Planning
First things first: every plan has to be built around the individual. A personalized care plan is the cornerstone. This is not some generic checklist. It's a detailed blueprint created just for your loved one, taking into account their unique medical history, daily routines, personal tastes, and long-term health goals.
A well-defined plan is the backbone of managing any chronic illness. You can get a feel for how they work by looking at these practical treatment plan example templates. For a senior in Princeton, this plan would cover everything from specific dietary needs for their diabetes to gentle exercises for their arthritis, ensuring their care respects them as a person.
Meticulous Medication Management
For many seniors, juggling multiple prescriptions is a daily headache. One little mistake—a missed dose, the wrong pill, or a bad drug interaction—can snowball into a serious health crisis. That's why medication management is absolutely non-negotiable.
This is so much more than just sorting pills into a weekly organizer. It means:
- Reconciliation: Regularly going over all medications—prescriptions, over-the-counter drugs, and supplements—with a doctor or pharmacist to make sure nothing clashes.
- Scheduling: Creating a simple, clear schedule for when to take each medication.
- Monitoring: Keeping a close eye out for any side effects and reporting them right away.
- Reminders: Using simple systems, whether it’s a phone app or a friendly reminder from an in-home caregiver from NJ Caregiving, to make sure no dose is ever forgotten.
Proper medication management is a critical safety net. Studies show that adverse drug events are a major reason why older adults end up in the hospital, making this pillar essential for preventing emergencies.
Continuous Monitoring and Communication
Chronic conditions are rarely static; they can shift and change over time. A small jump in blood pressure or a subtle change in breathing might seem insignificant, but they can be early warning signs of a brewing problem. That’s why continuous monitoring and open communication are so vital.
This means keeping track of key health numbers on a regular basis, like:
- Vital Signs: Blood pressure, heart rate, breathing rate, and temperature.
- Specific Metrics: Blood sugar levels for someone with diabetes or daily weight for a person with congestive heart failure.
- Symptom Journals: Simply noting any changes in pain, energy levels, or mood.
An in-home caregiver is perfectly positioned to notice these day-to-day changes. They become the crucial link between your loved one and their doctors, ensuring the entire medical team has the most current information to work with.
Patient and Family Education
Knowledge is power, plain and simple. For any of this to work, both the person with the condition and their family have to understand what’s going on, what the plan is, and what their role is. Patient and family education turns everyone from passive recipients of care into active, confident participants.
This education covers real-world skills, like how to properly use a blood glucose meter, what the early signs of a COPD flare-up look like, or how to cook heart-healthy meals that still taste good. When a family in Hamilton understands why that low-sodium diet is so important for their mom's heart, they're far more likely to help her stick with it and see positive results.
Coordination of Care
Finally, coordination of care is the glue that holds all the other pieces together. It’s common for seniors with chronic illnesses to see a whole team of specialists—a cardiologist, a pulmonologist, their primary doctor—plus pharmacists and physical therapists. Without someone connecting the dots, care can get fragmented, leading to conflicting advice or redundant tests.
This pillar ensures every single member of the healthcare team is on the same page. A geriatric care manager or a lead nurse from an agency like NJ Caregiving often steps into this role, making sure the cardiologist’s advice lines up with the endocrinologist's plan. This seamless collaboration prevents critical details from falling through the cracks and ensures your loved one receives holistic, truly person-centered care.
Managing Common Chronic Conditions in Seniors
The theory behind chronic disease management is great, but what does it actually look like day-to-day? This is where the rubber meets the road. For the millions of seniors living with conditions like heart disease, diabetes, arthritis, or COPD, a well-thought-out management plan isn't just an idea—it's a lifeline.
When we connect the core parts of management to these common illnesses, we start to see how this approach directly boosts a senior's quality of life. For families, this understanding is a game-changer. It turns complex medical advice into a series of clear, manageable actions that protect your loved one’s health and keep them independent for as long as possible. Let's dig into how these strategies work in the real world.

Proactive Management for Heart Disease
Heart disease is still one of the biggest health worries for older adults, but consistent, proactive management can make a world of difference. A smart plan doesn't just react to chest pain or high blood pressure readings; it works to keep things stable and prevent problems before they start.
Take a senior managing hypertension, for example. It’s about so much more than just remembering to take a pill. Real management involves:
- Daily Blood Pressure Monitoring: A caregiver can help track the numbers, spot any worrying trends, and get in touch with the doctor before a small issue becomes a big one.
- Dietary Support: Let's be honest, sticking to a low-sodium diet is tough. Having help with grocery shopping and meal prep is often the key to making it work.
- Medication Adherence: It’s not just about taking the medicine, but taking it at the right time, every single day, to keep blood pressure steady.
Cardiovascular diseases are a huge global concern, making up a massive 30.6% share of the chronic disease management market. The United Nations even set a goal to slash deaths from these conditions, as heart disease alone is responsible for half of those fatalities. Here in Hamilton and Princeton, in-home nursing support from providers like NJ Caregiving is crucial for monitoring vitals and preventing scary hospital readmissions after a cardiac event. For a deeper look into this kind of specialized care, check out our guide on congestive heart failure home care.
A Comprehensive Approach to Diabetes
If you want a perfect example of a holistic chronic care strategy, look no further than diabetes management. It’s a constant balancing act between medication, diet, and monitoring that requires daily, sometimes hourly, attention.
A successful diabetes management plan is like a three-legged stool—it needs medication, diet, and monitoring to stay balanced. If one leg is weak, the entire structure becomes unstable.
Keeping that stool steady takes a coordinated effort:
- Consistent Blood Sugar Checks: Regular testing isn't just about poking a finger; it's about gathering the data needed to make smart choices about insulin, meals, and exercise.
- Specialized Foot Care: Because of nerve damage, a senior might not feel a small cut or sore on their foot until it becomes a serious infection. Daily checks are non-negotiable.
- Meal Planning and Preparation: Helping a loved one navigate the tricky world of carbs and sugars ensures their blood sugar stays as stable as possible all day long.
Supporting Seniors with Arthritis and COPD
For conditions like arthritis and COPD that directly impact mobility and breathing, the focus of management shifts to maintaining function and maximizing comfort.
With arthritis, the main goals are to manage pain and keep joints as flexible as possible. This could mean helping with prescribed physical therapy exercises, making sure the home is free of trip hazards, and lending a hand with daily tasks that have become painful, like buttoning a shirt or opening a jar.
For someone with COPD, a caregiver can be on the lookout for the early signs of a flare-up, like worsening shortness of breath. They can also ensure that inhalers and any necessary oxygen equipment are being used correctly and consistently.
For seniors juggling these or other chronic health issues, knowing your Medicare Supplement insurance options is vital for covering the costs that Original Medicare doesn't. At the end of the day, chronic disease management is all about creating a supportive and structured environment. It’s about giving a senior the tools and help they need to live the fullest life possible, no matter what health challenges they face.
The True Benefits: Reduced Hospitalizations and Enhanced Quality of Life
While it’s helpful to know the moving parts of chronic disease management, what really matters are the life-changing results. This isn’t just about checking boxes or managing symptoms; it’s about giving seniors back a sense of stability, comfort, and independence.
The benefits show up in hospital records, but they’re also felt in the quiet, everyday moments at home.
The most dramatic, measurable outcome is a sharp drop in preventable hospital visits. Every symptom that’s kept under control and every medication mistake that’s avoided is a potential crisis averted—a crisis that would otherwise mean a stressful trip to the ER. Study after study confirms that coordinated care plans slash hospital readmission rates, particularly for tricky conditions like heart failure and COPD.
For families, this means fewer frantic, middle-of-the-night phone calls and less time spent anxiously waiting in a hospital. It fosters a predictable, secure environment where everyone can finally relax.
Beyond the Hospital Walls: Improving Daily Life
Keeping a loved one safe and out of the hospital is a massive win, but the benefits don’t stop there. Good chronic disease management has a direct impact on a senior’s day-to-day quality of life.
- Better Symptom Control: Consistent, proactive care helps manage chronic pain, fatigue, or shortness of breath. This makes it easier to enjoy simple activities and feel more comfortable throughout the day.
- Less Anxiety and Stress: Just knowing there’s a solid plan and a watchful caregiver brings incredible peace of mind, not just for the senior but for the entire family.
- Holding Onto Independence: By managing health challenges proactively, seniors are empowered to handle daily tasks, stay connected to their hobbies, and remain in the familiar comfort of their own homes.
What is chronic disease management if not a tool for empowerment? It’s about shifting the focus from simply surviving with an illness to actively thriving despite it, preserving dignity and personal choice.
A Hamilton Story: From Crisis to Comfort
Think about Robert, a 78-year-old from Hamilton struggling with severe COPD. His life had become a revolving door of ER visits. A minor cold could quickly escalate, leaving his family feeling helpless and constantly on edge, waiting for the next crisis.
Everything turned around when they put a structured in-home care plan in place with NJ Caregiving. A dedicated caregiver started monitoring Robert's oxygen levels, made sure he was using his inhalers correctly, and guided him through gentle breathing exercises.
When the caregiver noticed the very first signs of a respiratory infection, they didn't wait. They immediately coordinated with his doctor, who started him on antibiotics at home.
The result? Robert’s hospitalizations for COPD plummeted from six in one year to just one. He was strong enough to start enjoying his garden again, and his family could finally breathe a collective sigh of relief. This is what it's all about—turning a constant cycle of crisis into a story of stability and renewed life.
How In-Home Care Elevates Chronic Disease Management
A doctor's care plan is the roadmap, but professional in-home care is what gets the journey started. Think of it this way: a physician is like an architect who draws up a detailed blueprint for a healthier life. An in-home caregiver is the skilled builder who shows up every day to put that plan into action, turning instructions into consistent, daily habits.
They are the essential "boots on the ground" who bridge the gap between clinical advice and the realities of daily living. This is where the true power of chronic disease management unfolds. With a trained professional in the home, the plan is followed with precision, and small issues get caught before they snowball into major health crises.

From Daily Assistance to Skilled Nursing
In-home care isn't a one-size-fits-all service. It's a spectrum of support, customized to meet the specific needs outlined in a chronic disease management plan. For many seniors, this starts with a little help with the Activities of Daily Living (ADLs).
This kind of support helps older adults conserve energy and reduce their risk of falls or exhaustion, preserving both their dignity and independence. These services often include:
- Personal Care: Assistance with bathing, dressing, and grooming.
- Meal Preparation: Ensuring nutritious meals that align with dietary needs (like low-sodium or diabetic-friendly).
- Mobility Support: Helping a loved one move safely around the home.
When medical needs get more complex, skilled nursing services become crucial. A registered nurse (RN) or licensed practical nurse (LPN) from NJ Caregiving can provide clinical care right at home—things like wound care, managing complex medication schedules, and monitoring vital signs. You can learn more about these services in our guide on what are home health services.
When you're trying to decide what's best, it can be helpful to see the differences side-by-side.
In-Home Care Services vs Self-Management
| Management Task | Self-Management / Family Care | Professional In-Home Care (NJ Caregiving) |
|---|---|---|
| Medication Adherence | Can be inconsistent; relies on memory or family availability. | Trained professionals ensure correct dosages at the right times. |
| Monitoring Symptoms | Small changes might be missed or misinterpreted by family. | Caregivers are trained to spot early warning signs and report them. |
| Dietary Management | Meal prep can be overwhelming for families; mistakes are common. | Ensures meals meet specific dietary guidelines consistently. |
| Emotional Support | Family burnout is a real risk; can strain relationships. | Provides compassionate companionship and social engagement. |
| Coordination | Juggling appointments and information can be chaotic for family. | Acts as a central point of contact, coordinating with providers. |
Relying on family is a noble effort, but the consistent, trained support of a professional makes a world of difference in managing a chronic condition effectively.
More Than Just Medical Support
A chronic illness can be incredibly isolating. Loneliness itself poses significant health risks, often leading to depression and a faster decline in health. That’s why companionship is such a core piece of what we do.
A caregiver provides social interaction, engaging conversation, and emotional support that directly combats the health risks of isolation. This human connection is just as vital to a person's well-being as any medication reminder.
In-home care addresses the whole person, not just the disease. It recognizes that emotional well-being and social connection are critical pillars of a successful long-term management plan.
This support also extends to the rest of the family. Caring for a loved one with a chronic condition is demanding, and caregiver burnout is a real danger. Respite care gives family caregivers a much-needed break to rest and recharge, knowing their loved one is in capable, caring hands. This relief is essential for sustaining the family's ability to provide support for the long haul.
The Future of Managing Chronic Conditions
The role of in-home care is becoming more central to modern healthcare every day. It's poised to revolutionize chronic disease management, showing the fastest growth as the senior population—expected to reach 2.2 billion people over 65 by the 2070s—overwhelmingly prefers to age in place.
The market for these treatments is projected to grow from $9.74 billion in 2025 to $38.02 billion by 2034. This shift is powered by technologies like telehealth that allow for constant monitoring without frequent clinic visits. After a hospital stay, discharge planners increasingly rely on these services to reduce readmissions. In Mercer County, NJ Caregiving’s skilled professionals deliver this vital support, improving safety and overall well-being.
Ultimately, professional in-home care acts as an indispensable partner for families. It ensures a doctor's plan is executed faithfully every day, leading to better health, fewer hospital trips, and a richer quality of life for your loved one.
Funding Your Home Care Plan in New Jersey
Figuring out the financial side of care is one of the most important—and often most stressful—steps for families. The thought of paying for a chronic disease management plan with in-home care can feel overwhelming, but New Jersey actually has several clear pathways to make it affordable.
When you understand the options available, you can build a sustainable financial strategy. This ensures your loved one gets the consistent, high-quality support they need without putting a strain on your family.
Exploring Your Payment Options
Most families find that their funding comes from one of three main areas. Sometimes, a combination of these resources works best.
Navigating the payment landscape is much simpler once you know what to look for. Here are the most common ways to fund in-home care in New Jersey:
- Private Pay: This is the most direct route, where you pay for services out-of-pocket. It gives you the greatest flexibility to pick and choose the exact services and schedule you need, with no outside restrictions.
- Long-Term Care Insurance: If your loved one has a long-term care insurance policy, it’s usually designed specifically to cover services like in-home support for chronic conditions. We can help you make sense of your policy’s benefits and even assist with the paperwork to get claims started.
- Medicaid: For seniors who qualify, New Jersey Medicaid is an incredible resource. It provides significant support for in-home care, helping many people avoid or delay moving into a nursing home.
Leveraging New Jersey Medicaid for Home Care
New Jersey's Medicaid program is a lifeline for so many families. Through its Home and Community-Based Services (HCBS) waiver programs, Medicaid can cover a whole range of non-medical services that are absolutely essential for managing a chronic illness at home.
For many seniors, Medicaid is the key to aging in place. It empowers them to receive the daily support they need to manage their health safely and comfortably in their own homes, preserving their independence and connection to their community.
These programs often cover personal care like help with bathing and dressing, preparing meals, light housekeeping, and just as importantly, companionship. At NJ Caregiving, we have years of experience working with Medicaid. We can walk you through the process, help you figure out eligibility, and show you how to maximize your benefits to build an in-home care plan that truly supports your loved one for the long haul.
Your Chronic Disease Management Questions Answered
Navigating the world of chronic disease management can feel like learning a whole new language. To make things a bit clearer, we’ve put together answers to some of the most common questions we hear from families just starting to explore in-home care.
When Should We Consider Professional In-Home Care for a Chronic Condition?
The simplest answer is this: when managing things on your own starts to feel overwhelming. It’s not about one big catastrophic event; it’s usually a series of small but telling signs. Are medications getting mixed up more often? Are daily tasks like bathing or making a simple meal suddenly a huge challenge? Have there been a few too many trips to the hospital lately?
Another critical sign is caregiver burnout. If you, as the primary family caregiver, are feeling completely drained, it's a signal that you need support. Bringing in a professional early on isn't giving up—it's a smart move that can prevent a crisis, improve your loved one's health long-term, and restore a sense of calm and stability at home.
How Is a Chronic Disease Management Plan Created for a New Client?
It all starts with a conversation. We believe a care plan can't be created from a template; it has to be built around the person. The process begins with a thorough, in-home assessment by one of our registered nurses or care managers. They’ll sit down with your loved one and your family to truly understand the whole picture.
We’ll look at the medical side of things—doctor’s orders, medication lists, health history—but we’ll also focus on the personal side. What are their daily routines? What do they enjoy? What makes them feel comfortable and secure? All this information helps us build a personalized roadmap for care, outlining everything from medication schedules and mobility assistance to meal prep that aligns with their health needs and personal tastes.
A truly effective care plan is never a static checklist. It must be dynamic and responsive, adapting to a person’s changing health and personal goals to provide meaningful, day-to-day support.
Can In-Home Care Help with Multiple Chronic Conditions at Once?
Absolutely. In fact, this is where professional in-home care really shines. It’s very common for seniors to be managing more than one chronic condition, and our caregivers are trained specifically for this reality.
A good care plan is holistic, meaning it looks at how different conditions affect each other. For example, a caregiver can prepare a meal that is both heart-healthy for hypertension and low-sugar for diabetes. In the same visit, they can monitor blood pressure and blood sugar levels, then help with physical therapy exercises for arthritis. This integrated approach is the key to managing complex health needs safely and effectively.
What Is the Difference Between Palliative Care and Chronic Disease Management at Home?
It's easy to confuse the two because both focus on comfort and quality of life, but their core goals are different.
Think of chronic disease management as a long-term strategy. The focus is on controlling symptoms, slowing down the progression of a disease, and helping someone live as fully and independently as possible, often for many years.
Palliative care, on the other hand, is a specialized medical approach aimed at providing relief from the symptoms and stress of a serious illness, at any stage of that illness and even alongside curative treatment. While all good chronic care has elements of comfort and symptom relief, formal palliative care is a specific medical specialty. Our team can help coordinate with your loved one's healthcare providers to ensure they receive this specialized support if and when it's needed.
Managing a chronic condition is a journey, and you don’t have to do it alone. The compassionate team at NJ Caregiving is here to create a personalized care plan that brings comfort, safety, and peace of mind to your family. Contact us today to learn how we can support your loved one at https://njcaregiving.com.