Bringing a loved one home from the hospital is a huge relief, but it can also be a little nerve-wracking. Your first thought is making sure they have the medical support they need to recover safely. This is exactly where Medicare home health benefits come in.
This powerful resource provides skilled medical care—like nursing and therapy—delivered right in the comfort of home, bridging the gap between a hospital stay and a full recovery.
Your Roadmap to Understanding Home Health Care

There’s something powerful about healing in a familiar place. It’s not just a nice-to-have; it's a huge part of the recovery process. In fact, nearly 90% of seniors would much rather age and recover in their own homes. The Medicare home health benefit is designed to make that happen by covering specific, medically necessary services ordered by a doctor.
Think of it as an extension of your doctor's office, but without the travel. Instead of you going to appointments, skilled professionals come to you. This kind of support is critical for managing health conditions and getting back on your feet after a hospital stay or injury.
The Role of Medicare in Home Health
In the United States, Medicare is the backbone of this type of care. It's not just another option—it's the dominant payer, covering a massive number of home health visits nationwide. Of the 12 million Americans getting home health care each year, about 86% are age 65 or older, which really shows how central Medicare is to senior care.
Medicare pays for approximately 42% of all home health visits, making it the largest single payer for these vital services. This just goes to show how essential these benefits are for millions of seniors.
This guide is here to clear up the confusion and give you confidence. We'll walk you through everything you need to know about Medicare home health benefits, including:
- Who qualifies for coverage and what the eligibility rules really mean.
- Which specific services are included in the benefits.
- What you can expect to pay (if anything) out of pocket.
- How to get started with a certified home health agency.
By the end, you'll have a clear roadmap to getting the care you or your loved one needs to thrive at home. You can also explore more about home health industry trends to see just how vital this service is becoming.
Who Qualifies for Home Health Care Coverage?
Figuring out if you qualify for Medicare home health benefits is the very first step. The rules can seem a little complicated at first, but they're really there to make sure the benefit goes to people who are actively recovering from an illness, injury, or managing a serious health condition. To get the green light, your doctor needs to certify that you meet a specific set of criteria.
Think of these requirements as a checklist. Your doctor has to confirm that you meet every single one before they can map out a plan of care for you. This isn't just about filling out forms; it's a careful process to ensure skilled care at home is truly the right medical path for you at this moment.
The Doctor's Critical Role
Your journey to getting home health care always kicks off with your doctor. They are essentially the gatekeeper for these benefits. Before anything can happen, you must be under the care of a doctor who will create and regularly review your plan for home-based services.
This is more than just a quick signature on a form. Your doctor has to officially certify that you need one or more of the qualifying services. You'll also need a face-to-face meeting with a physician (or another qualified professional like a nurse practitioner) either within the 90 days before your home health care starts or the 30 days after. This in-person visit is crucial for documenting your need for care.
Needing Skilled Medical Services
At its heart, the Medicare home health benefit is all about skilled care. That's a really important distinction. It means you have to need services that can only be performed safely and correctly by a licensed professional.
You must require one of the following on an intermittent (not constant) basis:
- Skilled nursing care: This covers things like wound care, IV infusions, or injections that require a registered nurse.
- Physical therapy: To help you regain movement and strength after an injury or surgery.
- Speech-language pathology services: To help with communication or swallowing issues.
- Occupational therapy: To help you get back to performing daily activities like dressing or bathing.
Once you qualify because you need one of these primary services, you can also get other support, like help from a home health aide. But here's the catch: you can't qualify for home health benefits if you only need personal care from an aide.
Understanding the Homebound Requirement
The word "homebound" trips a lot of people up and can cause some unnecessary stress. It absolutely does not mean you're under house arrest or can't ever leave your house. It's simply a medical status that describes how difficult it is for you to get out and about.
Think of being homebound like having a temporary "home base" for your recovery. It's not a permanent state but a reflection that leaving home requires a considerable and taxing effort due to your illness or injury.
To be considered homebound, you have to meet two conditions:
- Condition One: You either need help from another person or use medical equipment (like a walker, wheelchair, or crutches) to leave your home. OR, your doctor believes your health could get worse if you leave.
- Condition Two: It's a major challenge for you to leave your home, meaning your trips out are infrequent and for short periods.
This definition has built-in flexibility for important outings. You can still go to medical appointments, attend religious services, or even get a haircut without risking your homebound status. The key is that these trips aren't your normal routine and take a significant effort.
Finally, the agency that provides your care must be certified by Medicare, which guarantees they meet federal health and safety standards. The whole point of the homebound rule is just to confirm that getting care at home is a medical necessity for you right now, not just a matter of convenience.
What Services Medicare Actually Covers

Once you’ve confirmed you're eligible, the next big question is, "So what kind of help can I actually get?" The heart of the Medicare home health benefit is providing skilled medical care to help you recover from an illness, get back on your feet after an injury, or manage a complex health condition.
Think of it as a specialized medical team coming directly to you. This isn’t about general household help; it’s about delivering specific, professional treatments that are medically necessary for your recovery. The goal is to bring the same level of professional care you'd get in a clinic right into the comfort and familiarity of your own home.
The Foundation of Care: Skilled Services
The services Medicare covers are all about being therapeutic and restorative. They require the hands-on expertise of licensed healthcare professionals to be performed safely and correctly. This is the absolute cornerstone of the entire benefit.
Here are the main types of skilled care you might receive:
-
Skilled Nursing Care: This is provided on a part-time or intermittent basis by a registered nurse (RN) or licensed practical nurse (LPN). It covers a whole range of medical tasks, like changing wound dressings, administering IV drugs, giving injections, or teaching you how to manage a new diabetes diagnosis. To get a better handle on this, you can learn more about what skilled nursing care entails and how it truly supports at-home recovery.
-
Physical Therapy (PT): If you've had a fall, a joint replacement, or a stroke, a physical therapist can come to your home. They’ll work with you to regain strength, improve your mobility, and restore your balance through targeted exercises and hands-on treatment.
-
Occupational Therapy (OT): An occupational therapist's job is to help you safely get back to your daily activities, or "occupations." This could be anything from relearning how to get dressed on your own, preparing a simple meal, or just moving around your home safely after being sick.
-
Speech-Language Pathology Services: If an illness has affected your ability to speak, communicate clearly, or even swallow, a speech therapist provides the essential treatment you need to recover these vital functions.
It's critical to remember that you must have a need for at least one of these skilled services to get the ball rolling. Once you do, however, you may also qualify for other supportive services that round out your plan of care.
Additional Support Services
Once your doctor orders skilled care and you qualify, Medicare might also cover other services that support your recovery plan. These aren't standalone benefits—they're add-ons to a plan that already includes skilled nursing or therapy.
These extra services can include:
-
Medical Social Services: These services can help you with the social and emotional side of dealing with an illness. For instance, a social worker can connect you with helpful community resources or assist you and your family in coping with the stress of a diagnosis.
-
Home Health Aide Services: While you're receiving skilled care, a home health aide can step in to help with personal tasks like bathing, dressing, and using the bathroom. This is only covered when it's part of the bigger picture, alongside your skilled nursing or therapy services.
What Is Not Covered
It's really important to have clear expectations about what Medicare will and won't pay for. The home health benefit is designed for specific medical needs, not for general household support or long-term personal assistance.
It's helpful to view the benefit as a bridge to recovery, not a permanent solution for daily living assistance. It covers medical needs but not custodial or personal care that could be provided by someone without professional medical training.
The following services are not covered under the Medicare home health benefit:
- 24-hour-a-day care at home: The benefit is only for intermittent or part-time care.
- Meal delivery: Services like Meals on Wheels are not included.
- Homemaker services: This means things like shopping, cleaning, and doing laundry.
- Personal care: Help with bathing or dressing is only covered if you are also getting skilled care. It can't be the only service you need.
Understanding this key difference helps families plan properly. Many find a great solution by combining Medicare-covered services with private pay help or family support to create a complete and seamless care plan.
Medicare Home Health Services Covered vs Not Covered
To make it even clearer, let's break down what falls under Medicare's coverage versus what you'll likely need to pay for out-of-pocket. This side-by-side view can help you see exactly where the lines are drawn.
| Service Category | What's Covered by Medicare | What's Not Covered (Out-of-Pocket) |
|---|---|---|
| Nursing & Therapy | Part-time skilled nursing; physical, occupational, and speech therapy. | Full-time or 24/7 nursing care. |
| Personal Care | Bathing and dressing support from an aide (if you're also getting skilled care). | Personal care as the only service needed. |
| Home Support | Medical social services to connect you with community resources. | General housekeeping, shopping, and laundry services. |
| Nutrition | Patient education on dietary needs related to a specific medical condition. | Meal preparation or meal delivery services. |
Seeing the services laid out like this can make it much easier to anticipate your needs and budget accordingly, ensuring there are no surprises down the road.
Understanding the Costs of Your Care
Whenever you're looking at healthcare, the first question on everyone's mind is always the same: "What's this going to cost me?"
Let's get right to the best part about Medicare home health benefits: for anyone who qualifies, the core skilled services that Medicare sends to your home cost you exactly $0. That’s right. There's no copayment to worry about and no deductible you have to meet before the benefits kick in.
This means if your doctor says you need skilled nursing, physical therapy, or other covered services at home, Medicare picks up 100% of the tab for those professional visits. The system is set up this way so that money doesn't stand in the way of you getting the critical care you need to get back on your feet.
Think of it as an all-inclusive recovery plan delivered to your door. The most important services—the hands-on expertise from nurses and therapists—are completely paid for. This simple, direct approach lets you and your family put all your energy where it belongs: on your health and recovery.
The One Exception: Durable Medical Equipment
While all the skilled care visits are fully covered, there is one key area you need to know about: durable medical equipment (DME). This is the stuff your doctor orders for you to use at home, like a walker, a hospital bed, oxygen tanks, or a commode chair.
For these items, you are responsible for paying 20% of the Medicare-approved amount. This is your coinsurance payment. Medicare covers the other 80%, but you will have a small out-of-pocket expense for the equipment itself.
- Here's a quick example: Let's say your doctor orders a hospital bed. If Medicare's approved price for that bed is $800, Medicare will pay $640 (80%). You would be responsible for the remaining $160 (20%).
It's really important to double-check that both the company supplying the equipment and the specific items they provide are approved by Medicare. This will guarantee you get the coverage you expect. To get a better handle on what you might pay, you can read our guide on decoding the cost of home health care, which breaks it all down even further.
How Medicare Pays for Your Care
It can also be helpful to understand a little bit about what's happening behind the scenes. Instead of paying for every single visit one by one, Medicare pays home health agencies in 30-day blocks of care. This approach is part of a system called the Patient-Driven Groupings Model (PDGM).
This model was created to put the focus squarely on your specific health needs, not just on how many visits an agency can rack up. When you start care, the agency builds a plan tailored to your condition. At the end of each 30-day period, they review your progress to see if you need to continue.
The switch to a 30-day payment system encourages agencies to provide care that's efficient and goal-oriented. It makes sure your care plan is always adapting to how you're actually doing.
The Centers for Medicare & Medicaid Services (CMS) is always tweaking this system to keep it effective. For example, they regularly update the payment rates to ensure everything stays fair and sustainable. This financial structure is why your care plan is constantly being reviewed and recertified—it’s all designed to make sure the services you're getting are medically necessary and actually working for you.
Your Step-By-Step Guide to Starting Services
Knowing you’re eligible for Medicare home health benefits is a huge relief, but actually getting the care started can feel like a whole new challenge. The good news is the process isn’t as complicated as it seems. It’s a structured path designed to get you the right support, fast.
Think of it as a coordinated effort between you, your doctor, and a home health agency to build a personalized recovery roadmap right in the comfort of your own home.
The entire journey kicks off with the most important person on your care team: your doctor. They are the official starting point for activating your benefits. This isn't just a formality—it’s a critical step to ensure the care you receive is medically necessary and tailored specifically to your health needs.
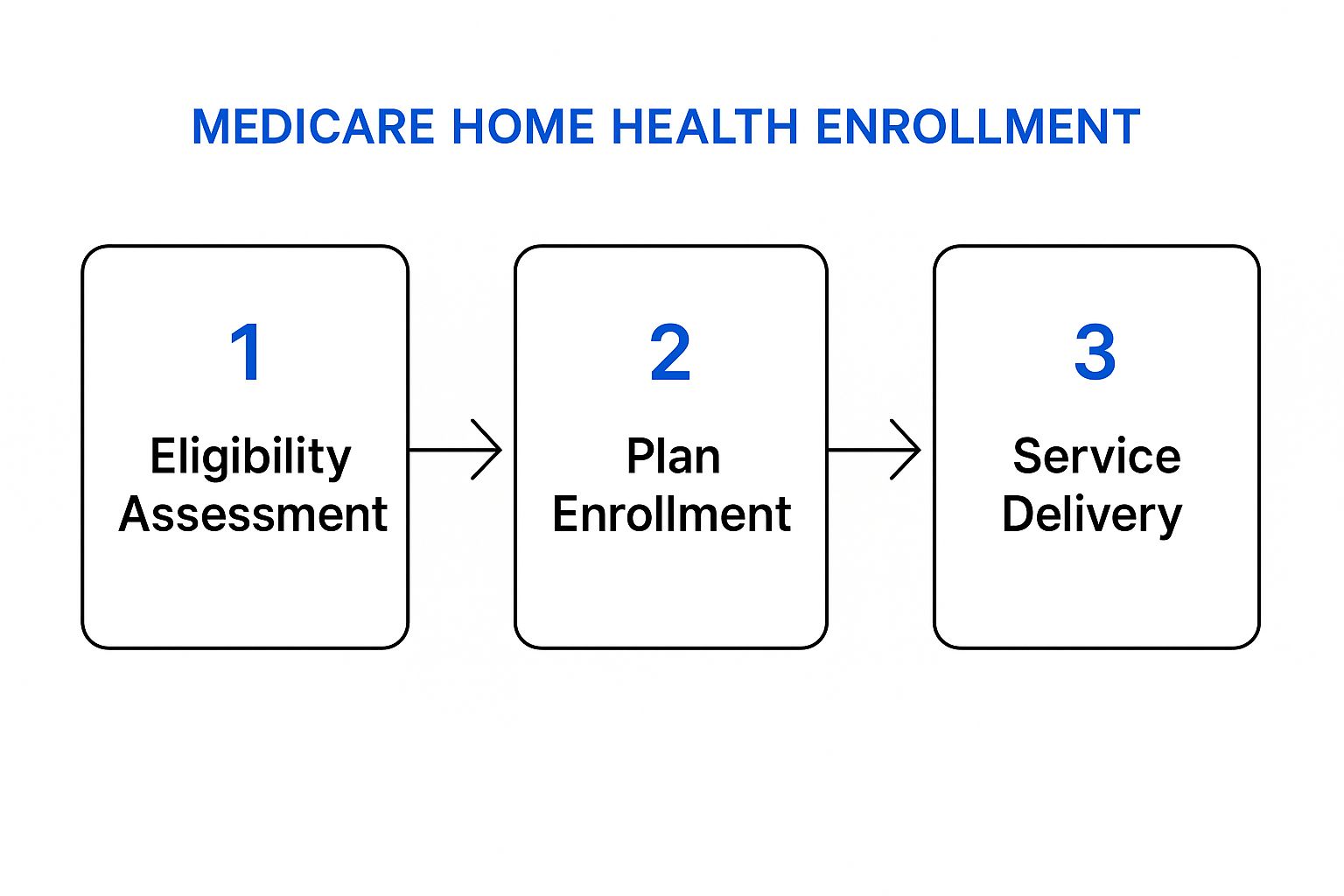
This visual breaks it down nicely, showing the clear, three-step progression from a doctor's confirmation of your needs to receiving skilled care where you're most comfortable.
Step 1: The Doctor’s Referral and Certification
Your path to home health care always starts with your physician. After a thorough assessment of your condition, your doctor must officially certify that you meet all of Medicare’s eligibility criteria, including being homebound and needing skilled care.
This certification is formalized in a document called a plan of care. It essentially acts as the prescription for your home health services. It will detail the types of care you need (like physical therapy or skilled nursing), how often you need them, and what health goals you’re working toward. This initial plan is the blueprint for everything that follows.
Step 2: Finding a Medicare-Certified Agency
With your doctor's orders in hand, the next step is choosing a home health agency. This is a crucial choice, and you have the right to select any agency that is certified by Medicare. An agency earns this certification by meeting strict federal health and safety standards, which is your assurance that you’ll receive high-quality, professional care.
You’re not alone in this search. Medicare provides a powerful online tool to help you find and compare agencies in your area.
-
Use the Care Compare Tool: This official Medicare website lets you search for certified agencies by zip code. You can see how agencies stack up based on patient satisfaction surveys and quality-of-care metrics.
-
Ask for Recommendations: Your doctor's office, a hospital discharge planner, or even a local senior resource center can often provide a list of reputable local agencies they’ve worked with before.
-
Interview Potential Agencies: Don’t hesitate to call a few agencies and ask questions. A good agency will be happy to walk you through its services, staffing, and overall approach to care.
Choosing an agency is like hiring a partner for your recovery. It’s important to find a team that not only meets high clinical standards but also communicates well and makes you feel comfortable and respected.
Step 3: Developing Your Official Plan of Care
Once you've picked an agency, they will schedule an initial visit to your home. A registered nurse or therapist will come out to conduct a comprehensive assessment. They’re not just looking at your primary diagnosis; they'll evaluate your overall health, living situation, and any safety needs you might have.
This detailed evaluation is often documented on a specific form. You can get a better idea of what's involved by looking into what a typical home health care assessment form includes.
Based on this in-depth assessment and your doctor’s orders, the agency finalizes your official plan of care. This document becomes the master guide for your treatment and will be regularly reviewed and updated by your doctor at least once every 60 days.
The plan of care will clearly outline:
- The specific services you'll receive (e.g., skilled nursing, physical therapy).
- The frequency and duration of the visits from each professional.
- The medical equipment you may need, such as a walker or hospital bed.
- The specific goals of your treatment, like being able to walk unassisted to the mailbox.
From this point forward, the agency will coordinate all visits and work directly with your doctor to manage your care, making sure you’re on a steady path to recovery.
Seeing Home Health Care in Action

It’s one thing to read the rules for Medicare home health benefits, but it’s another thing entirely to see how they come to life. These benefits aren't just policies on a page; they're the support system that helps people get back on their feet in the place they feel most comfortable—home.
Let's move past the technical definitions and walk through a few common situations. Seeing how a real plan of care comes together shows you exactly what kind of skilled services are involved and how someone actually meets the eligibility requirements.
Scenario 1: Recovering from Joint Replacement Surgery
Picture Maria, a 72-year-old who just had a total knee replacement. The hospital has discharged her, but she’s far from independent. She can't drive, and her mobility is seriously limited, making it a major struggle just to leave the house. This makes her officially homebound.
Her doctor sets up a plan of care designed to get her strength and independence back safely. This plan is what kicks her Medicare home health benefits into gear.
Her care team would likely look something like this:
- A physical therapist comes to her home three times a week. They work with her on exercises to improve her knee's range of motion, build back her leg strength, and practice getting around with a walker.
- An occupational therapist visits once a week to help her adjust her daily routines for safety. This could mean installing a shower chair, showing her how to get dressed without straining her new knee, or figuring out how to safely make a meal in her kitchen.
- A skilled nurse stops by at the beginning of her recovery to check the surgical incision for any signs of infection, make sure her pain medication is working correctly, and go over her recovery instructions.
In Maria’s case, her clear need for skilled therapy was the key that unlocked all of her benefits, with the skilled nurse providing that extra layer of medical oversight.
Scenario 2: Managing Chronic Heart Failure
Now, let's think about Robert, an 80-year-old who lives with chronic congestive heart failure (CHF). He was recently in the hospital for shortness of breath, and his condition is still shaky. His doctor certifies that he needs skilled monitoring at home to keep him from ending up back in the hospital.
For chronic conditions like CHF, home health care is a proactive tool. It’s not just about reacting to a crisis; it’s about providing consistent, skilled oversight to manage symptoms and keep the patient stable at home.
Robert's care plan focuses on long-term disease management. A skilled nurse visits him twice a week to:
- Track his weight, blood pressure, and oxygen levels.
- Check for swelling in his legs and feet, a common sign of trouble.
- Educate both him and his wife on his low-sodium diet and complex medication schedule.
This steady nursing care helps catch potential issues before they become emergencies, dramatically cutting down the odds of another stressful and expensive hospital stay.
Scenario 3: Navigating Dementia Care at Home
Caring for someone with dementia brings a whole different set of challenges. It's no surprise that research consistently shows that patients with dementia use home health services at higher rates than those without. Factors like age, gender, and being eligible for both Medicare and Medicaid are also tied to higher use, which really speaks to the complex needs of this group. You can discover more insights on home health trends for dementia patients in recent studies.
Take Susan, a 78-year-old with moderate Alzheimer's. After a fall, her doctor orders home health services to help her stay safe. A speech-language pathologist works with her on memory and communication exercises, while a physical therapist focuses on improving her balance to prevent another fall.
Under the supervision of a registered nurse, a home health aide also comes in to help with tasks like bathing, which has become too difficult and unsafe for Susan to handle on her own.
Your Questions Answered: Making Sense of Home Health Benefits
When you start digging into the details of Medicare home health benefits, it's natural for a few practical questions to pop up. Getting a handle on how long you can receive care, what the rules really mean, and what your rights are is the first step toward feeling confident about your recovery plan.
Let’s clear up a couple of the most common things we hear from families.
How Long Can I Receive These Benefits?
This is a big one, and the answer is often a relief: there is no lifetime limit on Medicare home health benefits.
As long as you continue to meet all the eligibility rules, your doctor can simply recertify your plan of care every 60 days. This is just a regular check-in to confirm that the skilled services you're receiving are still medically necessary for your condition.
Can I Still Work and Be Considered Homebound?
The "homebound" rule can feel a little confusing, but it's pretty strict. It generally means that leaving your home takes a major, taxing effort. Because of this, if you're able to work outside the home, you most likely won't meet this specific requirement.
That said, Medicare understands you can't be completely isolated. Brief and infrequent trips for non-medical reasons, like attending a religious service, are perfectly fine.
If your claim for home health care is denied for any reason, you have the right to appeal. The agency must give you a written notice that explains why and provides clear instructions on how to start your appeal right away.
At NJ Caregiving, we believe that clear information is the best tool for making health decisions. If you're in Mercer County and need compassionate, skilled in-home care, we'd be honored to show you how our team can support your recovery. Find out more at https://njcaregiving.com.


