It’s a huge myth that poor sleep is just a normal part of getting older. While it’s true that sleep patterns can change over time, constant trouble falling asleep, waking up all night, or feeling exhausted all day are usually red flags for treatable sleep disorders in elderly adults—not something you just have to accept. Getting to the bottom of these issues is a game-changer for health and happiness.
The Overlooked Challenge of Senior Sleep
For too many seniors and the people who care for them, restless nights and groggy days are the norm. The old belief that "older people just don't sleep well" often stops them from getting help for what are real, manageable medical conditions. This isn't just an outdated idea; it's a dangerous one. Quality sleep is absolutely fundamental to aging well.
Think of deep, restorative sleep as your body's nightly tune-up crew. It's when the brain organizes memories, cells get repaired, and energy stores are refilled for the next day. When sleep disorders constantly interrupt this vital work, the fallout can be serious.
Why Prioritizing Sleep is Crucial
Brushing off poor sleep can trigger a whole host of health problems that go way beyond just feeling a bit tired. For seniors, getting enough good-quality sleep is directly tied to:
- Cognitive Function: Deep sleep is essential for sharp thinking and solid memory recall. Not getting enough can actually look like—or even worsen—symptoms of cognitive decline.
- Emotional Stability: A sleep-deprived brain is often a more irritable and anxious one. It lowers the ability to handle stress and can take a toll on mood and relationships.
- Physical Safety: Feeling drowsy during the day is a major risk factor for falls, which can lead to devastating injuries. A senior who is well-rested is naturally more alert, stable, and safe.
This is a massive issue. Studies show that about half of all adults over 60 struggle with poor sleep, making this a major health concern around the world. You can take a deeper dive into the numbers and what they mean by reading the full study.
This isn't just about feeling tired; it's about preserving independence, cognitive health, and overall well-being. Recognizing that persistent sleep problems are a medical issue—not a normal part of aging—is the first step toward finding effective solutions.
Moving from Myth to Action
Once seniors and their caregivers understand that sleep disorders in elderly people are real medical problems, they can start taking action. Instead of just putting up with sleepless nights, the goal is to find out what’s causing them. This guide will walk you through how to spot the warning signs of common disorders, look at effective treatments, and use practical tips to finally get some rest. By changing the conversation, we can shift from just accepting the problem to actively solving it.
Why Sleep Patterns Change With Age

Have you ever noticed your internal alarm clock seems to be set completely differently than it was years ago? Maybe you feel tired much earlier in the evening or find yourself wide awake long before the sun is up. These shifts aren't just in your head—they're rooted in real, biological changes that come with getting older.
Think of your body's internal clock, the circadian rhythm, like a finely tuned vintage watch. For decades, it kept perfect time, guiding your sleep and wake cycles with incredible precision. As the years pass, that watch can lose some of its accuracy. It’s not broken, but it might run a bit fast or need more careful winding.
This natural drift of your internal clock is a big reason why sleep patterns change with age. While it’s a normal part of life, understanding what’s happening is the first step toward managing the sleep disorders in elderly adults that can sometimes follow.
The Biology Behind Shifting Sleep
A few key physiological factors are at play here, and one of the biggest is a change in hormone production. Your brain naturally produces a hormone called melatonin to signal that it's time to sleep.
As we get older, the gland that makes melatonin becomes less efficient and releases smaller amounts. This means the "time for bed" signal gets weaker, which can make it harder to fall asleep and stay asleep all night.
This shift in the sleep-wake cycle is known as an advanced sleep phase. It’s why many older adults feel sleepy early in the evening (say, 8 or 9 PM) and wake up very early in the morning (like 4 or 5 AM). While not a disorder on its own, it can throw a wrench in social plans and lead to daytime fatigue if you’re not prepared for it.
Another fundamental change happens to the very structure of our sleep. Sleep isn’t just one long state of rest; it's made up of different stages, including light sleep, deep sleep, and REM (dream) sleep. Deep sleep is the most physically restorative stage—it’s when the body does most of its heavy lifting for repair and recovery.
Unfortunately, the amount of time seniors spend in this crucial deep sleep stage naturally shrinks. The result is sleep that’s lighter and more easily disturbed, which contributes to that frustrating feeling of not being well-rested, even after a full night in bed.
How Health Conditions Interrupt Sleep
Of course, these biological changes don't happen in a vacuum. They are often made worse by age-related health conditions that can create a perfect storm for sleep disruption. As the body’s sleep architecture becomes more fragile, it's more vulnerable to being disturbed, and new or chronic health issues are often the culprits.
Common issues that can fragment sleep include:
- Chronic Pain: Conditions like arthritis can make it tough to get comfortable, leading to frequent wake-ups every time you shift.
- Bladder Issues: The need to use the bathroom more often at night, a condition known as nocturia, can break sleep into short, unsatisfying chunks.
- Breathing Problems: Conditions such as heart failure or COPD can cause shortness of breath when lying down, forcing you awake suddenly.
- Medication Side Effects: Many common prescriptions for blood pressure, depression, and other conditions can interfere with sleep as an unfortunate side effect.
These interruptions prevent the brain from cycling through all the necessary sleep stages, further cutting down on that deep, restorative rest. This interplay between natural aging and health conditions is a key reason why sleep disorders in elderly individuals are so common.
For a broader look at proactive wellness, our senior health and wellness guide to aging gracefully offers valuable insights that support better sleep and overall vitality. By understanding these connected factors, both caregivers and seniors can get better at spotting the root causes of sleep problems and start finding effective solutions.
Identifying Common Senior Sleep Disorders
It's a common misconception that poor sleep is just a normal part of getting older. While sleep patterns certainly change with age, persistent and disruptive problems are often a red flag for a specific, treatable condition. The first step toward relief is simply knowing what to look for.
Think of this as a field guide to the most common sleep disorders in elderly adults. Spotting these warning signs in yourself or a loved one can make all the difference. These aren't just minor annoyances; they're genuine medical conditions that can seriously impact health and quality of life if ignored.
This chart highlights the primary triggers that can work together to throw a senior's sleep cycle off balance.
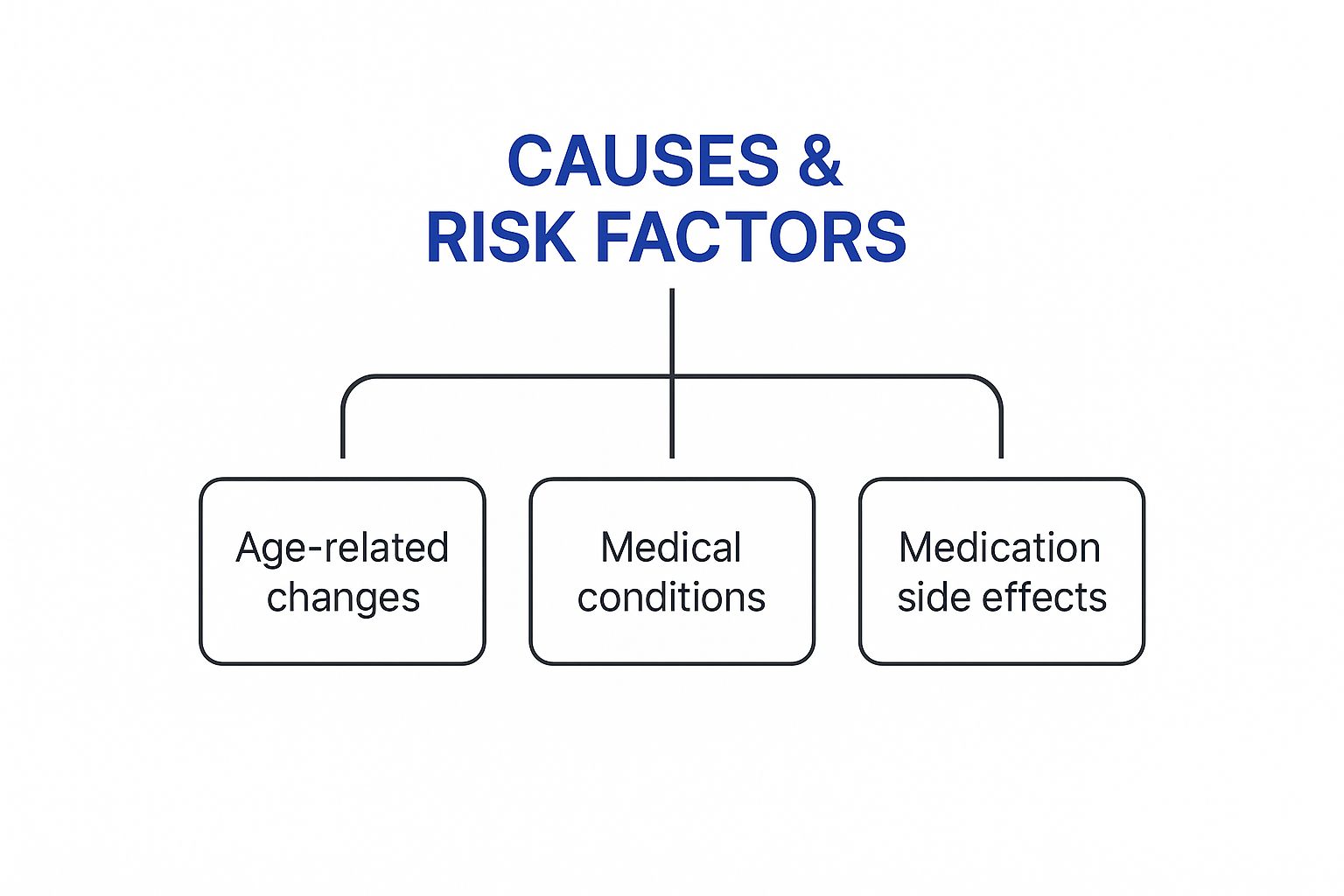
As you can see, biological shifts, existing health issues, and medication side effects often create a perfect storm for sleep disruption.
To help you tell these conditions apart, here is a quick comparison table outlining the key features of each.
Comparing Common Sleep Disorders in Seniors
| Disorder | Primary Symptom | Key Characteristic | Primary Risk Factor |
|---|---|---|---|
| Insomnia | Difficulty falling/staying asleep | Waking up feeling unrefreshed | Age, other medical conditions |
| Obstructive Sleep Apnea | Pauses in breathing during sleep | Loud snoring, gasping for air | Obesity, age-related muscle changes |
| Restless Legs Syndrome | Uncontrollable urge to move legs | Symptoms worsen at rest/night | Iron deficiency, certain medications |
| REM Sleep Behavior Disorder | Physically acting out dreams | Lack of normal muscle paralysis | Early sign of neurodegenerative disease |
This table provides a snapshot, but understanding the nuances of each disorder is crucial for recognizing them in daily life. Let's dig a little deeper into what each one looks and feels like.
Insomnia
Insomnia is the one we’ve all heard of. It’s the frustrating experience of not being able to fall asleep, stay asleep, or waking up way too early without being able to drift back off. For seniors, this isn't about a single bad night; chronic insomnia can become a daily battle that saps energy, dampens mood, and clouds thinking.
This condition is incredibly common, affecting up to 75% of older adults. It's often tangled up with other physical and psychiatric issues that come with age, making it even tougher to get that deep, restorative sleep the body needs.
The classic signs include:
- Lying awake for what feels like forever before finally falling asleep.
- Waking up over and over throughout the night.
- Feeling tired and groggy in the morning, even after a full night in bed.
- Daytime fatigue, irritability, and trouble concentrating.
When left untreated, chronic insomnia can increase the risk of falls, cognitive decline, and depression. The good news is that effective treatments exist. You can learn much more about managing insomnia in the elderly in our detailed guide.
Obstructive Sleep Apnea
Obstructive Sleep Apnea (OSA) is a serious disorder where a person's breathing repeatedly stops and starts all night long. Think of the airway as a soft, flexible tube. With OSA, the throat muscles relax too much during sleep, causing this tube to collapse and completely block airflow.
The brain quickly senses the drop in oxygen and sends out a panic signal, jolting the person partially awake to reopen their airway—often with a loud gasp or snort. This can happen hundreds of times a night without the person ever consciously realizing it, preventing them from ever reaching the deeper stages of sleep.
Loud, chronic snoring is the hallmark sign, but OSA is so much more than a noisy habit. Each pause in breathing puts a massive strain on the heart and blood vessels, raising the risk for high blood pressure, heart attack, and stroke.
Key signs to watch for include:
- Loud, persistent snoring that disrupts others.
- Someone else noticing pauses in their breathing while they sleep.
- Abrupt awakenings where they feel like they are choking or gasping.
- Feeling exhausted during the day, no matter how long they were in bed.
- Waking up with a headache or a very dry mouth.
Restless Legs Syndrome
Restless Legs Syndrome (RLS), sometimes called Willis-Ekbom disease, is a neurological condition that creates an irresistible, overwhelming urge to move the legs. The sensation is often described as a strange creepy-crawly, pulling, or throbbing feeling deep inside the limbs.
The defining trait of RLS is that the symptoms are always worse at night when someone is resting, especially when they lie down to go to sleep. The only thing that brings temporary relief is movement—stretching, walking, or shaking the legs. This constant need to move makes it nearly impossible to fall asleep and stay asleep.
While the exact cause isn't always known, RLS is often connected to iron deficiency, certain medications, and other health conditions common in seniors, like kidney disease or diabetes.
REM Sleep Behavior Disorder
REM Sleep Behavior Disorder (RBD) is a dramatic and potentially dangerous condition where a person physically acts out their dreams. During the REM (Rapid Eye Movement) stage of sleep—when our most vivid dreams happen—the body normally goes into a state of temporary muscle paralysis. It’s a brilliant safety feature that stops you from actually running from the monster in your dream.
In someone with RBD, that paralysis mechanism fails. As a result, they might shout, punch, kick, or even leap out of bed in response to their dream. This can lead to serious injuries, both for them and for anyone sleeping next to them.
RBD is often considered an early warning sign for neurodegenerative diseases like Parkinson's or Dementia with Lewy Bodies. If you notice these symptoms, it’s a clear signal to seek a thorough medical evaluation. Recognizing these distinct sleep disorders in elderly loved ones is the essential first step toward getting a diagnosis and creating a plan for safer, more restful nights.
Navigating Diagnosis and Professional Treatment

Suspecting a sleep disorder is the first step, but getting from suspicion to a solid diagnosis and treatment plan is where the real change happens. This journey almost always starts with a conversation with a doctor, and being prepared for that chat can make all the difference.
Before the appointment, it’s a great idea to keep a sleep diary for a week or two. Think of it as gathering clues. This log doesn’t have to be complicated—it’s just a simple, daily record of their sleep patterns.
Try to note down key details like:
- What time did they go to bed?
- Roughly how long did it take to fall asleep?
- How many times did they wake up during the night?
- What time did they finally get up for the day?
- Did they nap? If so, for how long?
- How did they feel the next day? (e.g., groggy, refreshed, irritable)
This simple record gives a doctor a clear picture of the problem, turning vague complaints like "I'm not sleeping well" into concrete data. It helps uncover patterns that might point toward specific sleep disorders in elderly adults.
The Diagnostic Process Explained
Based on the sleep diary and your conversation, a doctor might suggest a more detailed investigation. One of the most common and definitive diagnostic tools is an overnight sleep study, professionally known as a polysomnography.
This might sound intimidating, but it’s a completely painless process. The senior spends a night in a comfortable, private room at a sleep center while small sensors monitor various bodily functions.
These sensors keep track of important metrics such as:
- Brain wave activity
- Eye movements
- Heart rate and rhythm
- Breathing patterns and oxygen levels
- Leg movements
All this data gives specialists a behind-the-scenes look at what’s really happening when sleep gets disrupted. It’s the key to an accurate diagnosis of conditions like sleep apnea or REM Sleep Behavior Disorder.
Exploring Modern Treatment Solutions
Once a diagnosis is confirmed, the focus shifts to finding the right treatment. It’s important to know that modern solutions for sleep disorders in elderly individuals go way beyond just prescribing sleeping pills. Today's treatments are often multi-faceted, blending lifestyle adjustments with targeted medical interventions.
Many medications can also impact rest, so it's essential to have a clear list. Our guide on senior medication management can help you get this crucial information organized before speaking with a doctor.
CBT-I: The Gold Standard for Insomnia
For chronic insomnia, the first-line treatment recommended by experts isn't a pill at all. It's a type of therapy called Cognitive Behavioral Therapy for Insomnia (CBT-I). This approach is incredibly effective because it gets to the root causes of sleeplessness—the anxious thoughts and unhelpful habits that have built up around bedtime.
CBT-I helps people unlearn the negative patterns that are keeping them awake. It gives them the tools to calm their mind and retrain their body's natural sleep-wake cycle for good.
Instead of creating dependency, CBT-I provides lasting skills. It helps break that frustrating cycle of worrying about sleep, which is ironically the very thing keeping so many people awake.
Demystifying CPAP for Sleep Apnea
For Obstructive Sleep Apnea (OSA), the most common and effective treatment is Continuous Positive Airway Pressure (CPAP) therapy. The machine can look a bit intimidating at first, which causes some people to resist trying it. A simple analogy can help clear things up.
Think of the airway as a soft, collapsible straw. For someone with OSA, this straw collapses during sleep, blocking air. A CPAP machine uses a mask to send a gentle, steady stream of air that acts like an "air splint," keeping the straw propped open all night long.
This continuous pressure prevents those breathing interruptions, allowing the body to finally get the deep, restorative sleep it's been missing. And it's a significant concern—the prevalence of OSA in U.S. adults is estimated to be between 10% to 30%, with rates even higher among the elderly. You can discover more insights about sleep health on worldsleepday.org.
By understanding these diagnostic steps and treatment options, caregivers and seniors can face the problem with confidence, knowing that proven solutions are available to bring back restful nights.
Building a Better Bedtime Routine
Once you have a handle on the common sleep disorders that affect seniors, it's time to take action. While conditions like sleep apnea absolutely require professional medical treatment, improving daily habits can create a powerful foundation for better rest. This isn’t just about generic “sleep hygiene,” either. It’s about a thoughtful approach that keeps the specific needs and safety of older adults front and center.
Think of the body’s internal clock—its sleep-wake cycle—as a rhythm that needs consistent cues to stay on beat. A structured bedtime routine is like a conductor, signaling to the brain and body that it’s time to wind down and get ready for a restorative night. That consistency is what really reinforces the clock.
Creating a Safe and Soothing Sleep Environment
The bedroom should be a sanctuary for sleep, plain and simple. That means getting rid of distractions and potential hazards. For seniors, optimizing this space for both comfort and safety is critical, especially since waking up in the middle of the night is so common. You'd be surprised how a few small adjustments can make a huge difference in preventing falls and helping them get back to sleep.
Consider making a few of these simple environmental tweaks:
- Lighting: Plug in some dim, warm-toned nightlights in the bedroom, hallway, and bathroom. This gives just enough light to move around safely without the jarring shock of a bright overhead light, which can make it almost impossible to fall back asleep.
- Temperature: Keep the room on the cool side, somewhere between 60-67 degrees Fahrenheit. A cooler room helps trigger the body’s natural drop in core temperature, which is a key signal for sleep.
- Noise Control: If disruptive sounds are an issue, try earplugs, a white noise machine, or even a simple fan. This can mask sudden noises from traffic or a snoring partner that might otherwise break up their sleep.
- Bed Comfort: Make sure the mattress and pillows are actually comfortable and supportive. This is especially important if they’re dealing with chronic pain from conditions like arthritis.
Your bedroom should be for two things: sleep and intimacy. When you strengthen that mental connection, your body learns that getting into bed means it's time to rest. Removing TVs, tablets, and phones gets rid of stimulating blue light and the mental clutter that can sabotage a good night's sleep.
Establishing a Relaxing Pre-Sleep Ritual
A consistent pre-sleep ritual is a powerful cue to the brain that the day is officially over. This sequence of calming activities should start about 30 to 60 minutes before you want them to be asleep. The entire goal is to transition from the busyness of the day to a state of relaxation.
An effective routine could include a few of these steps:
- Dim the Lights: Lowering the lights throughout the house an hour or so before bed helps kickstart the body's natural melatonin production.
- Engage in Quiet Activities: Reading a real book (not on a screen!), listening to calming music, or working on a crossword puzzle can help quiet a racing mind.
- Practice Relaxation Techniques: Gentle stretching, some deep breathing exercises, or a guided meditation can release physical tension and ease away anxiety.
- Enjoy a Warm Beverage: A small, caffeine-free cup of herbal tea like chamomile or even a glass of warm milk can be wonderfully soothing.
Managing Diet and Hydration for Better Nights
What and when an older adult eats and drinks has a direct line to their sleep quality. You want to avoid anything that could cause discomfort or force them to get up during the night.
- Avoid large meals close to bedtime. A heavy meal can trigger indigestion or heartburn, making it tough to get comfortable. Try to have them finish dinner at least two to three hours before they lie down.
- Limit caffeine and alcohol. Both can seriously mess with sleep. Caffeine should be cut off at least six hours before bed. And while alcohol might make them feel sleepy at first, it often leads to waking up multiple times later in the night.
- Manage fluid intake. Staying hydrated is key, but encourage them to drink more fluids earlier in the day and taper off in the evening. This can minimize those nighttime trips to the bathroom.
Harnessing Daytime Habits for Nighttime Success
A good night's sleep doesn't just start at bedtime—it's built throughout the day. The habits they keep from the moment they wake up play a huge role in setting their internal clock and building up enough "sleep drive" to get them through the night.
Encourage these simple daily practices:
- Get Morning Sunlight: Getting some natural light within the first hour of waking is one of the best ways to set the body's circadian rhythm for the day.
- Stay Physically Active: Gentle, regular exercise like a daily walk or some chair yoga can significantly improve sleep quality. Just try to avoid anything too vigorous right before bed.
- Limit Naps: If a nap is needed, keep it short (20-30 minutes) and try to have it earlier in the afternoon. A long or late nap can make it much harder to fall asleep at night.
Frequently Asked Questions

When you're caring for an older loved one, navigating the world of sleep disorders in elderly adults can bring up a lot of questions. It's completely normal to feel a bit lost. We've gathered some of the most common concerns caregivers have and provided clear, straightforward answers to help guide you.
Think of this as your quick-reference guide for getting reliable information and clearing up any confusion about helping your loved one get better rest.
Are Over The Counter Sleep Aids Safe For Seniors?
It’s so tempting to grab a quick fix from the pharmacy shelf, but for older adults, most over-the-counter sleep aids can do more harm than good. A lot of these products contain diphenhydramine, an antihistamine that’s notorious for causing next-day confusion, dizziness, and a real sense of unsteadiness.
These side effects aren't just unpleasant; they dramatically increase the risk of falls, which can lead to devastating injuries. That's why it's absolutely critical to talk with a doctor before even considering any sleep aid.
A doctor will almost always start with safer, non-drug approaches. Cognitive Behavioral Therapy for Insomnia (CBT-I) is the gold standard for a reason—it gets to the root causes of sleeplessness without the risky side effects of medication, making it the most effective long-term solution.
How Do I Know If It Is Normal Aging Or A Sleep Disorder?
It’s true that sleep patterns change as we get older. Sleeping a bit lighter or waking up earlier isn't necessarily a cause for alarm. But a true sleep disorder is different—it actively disrupts daily life and well-being.
The real difference is in the consequences. If poor sleep consistently leads to debilitating daytime fatigue, irritability, memory lapses, or needing multiple naps just to function, you're looking at something more serious than just aging.
And some symptoms are never a normal part of getting older. If you notice any of the following, it’s time to seek medical advice right away:
- Loud, chronic snoring that’s punctuated by gasping or choking sounds.
- An uncontrollable urge to move the legs, especially when trying to rest at night.
- Physically acting out dreams by kicking, punching, shouting, or thrashing around.
These are classic signs of specific sleep disorders in elderly adults that need a professional diagnosis to be managed properly.
Can Lifestyle Changes Help A Serious Disorder Like Sleep Apnea?
When you’re dealing with a condition like moderate to severe sleep apnea, lifestyle changes on their own aren't going to be a cure. But that doesn't mean they aren't important—in fact, they are a crucial piece of the puzzle and can make a huge difference in the success of a treatment plan.
Simple adjustments can make medical treatments like CPAP therapy much more effective. For instance, maintaining a healthy weight helps reduce pressure on the airway, and steering clear of alcohol before bed keeps the throat muscles from becoming too relaxed.
Even something as simple as sleeping on your side instead of your back can physically help keep the airway from collapsing. These habits work hand-in-hand with prescribed treatments, helping to lessen the severity of breathing interruptions and boost overall sleep quality.
Navigating the challenges of elder care can feel overwhelming, but you don't have to do it alone. For compassionate, professional in-home support that prioritizes safety and well-being, trust NJ Caregiving. Learn more about our personalized services at https://njcaregiving.com.


