The core difference is simple: home health is skilled medical care that a doctor prescribes, while home care is non-medical support for daily living.
It’s the difference between a registered nurse managing post-surgery wound care and a friendly aide helping with meals, bathing, and companionship.
Decoding Home Health And Home Care At A Glance
Trying to figure out in-home support options can feel like a lot to take on, but once you understand the main purpose of each service, the choice becomes much clearer.
Home health care is clinical, usually temporary, and has specific goals. It's designed to help someone recover from an illness, an injury, or a recent hospital stay. These services have to be ordered by a physician and are always carried out by licensed medical professionals.
On the other hand, home care is all about maintaining a person's quality of life and independence by helping with Activities of Daily Living (ADLs). This kind of support is often for the long term and doesn't need a doctor's order. To get a better sense of what this involves, you can check out our detailed guide on non-medical home care options.
This image breaks down the key differences in cost, provider qualifications, and the complexity of care between home health and home care.
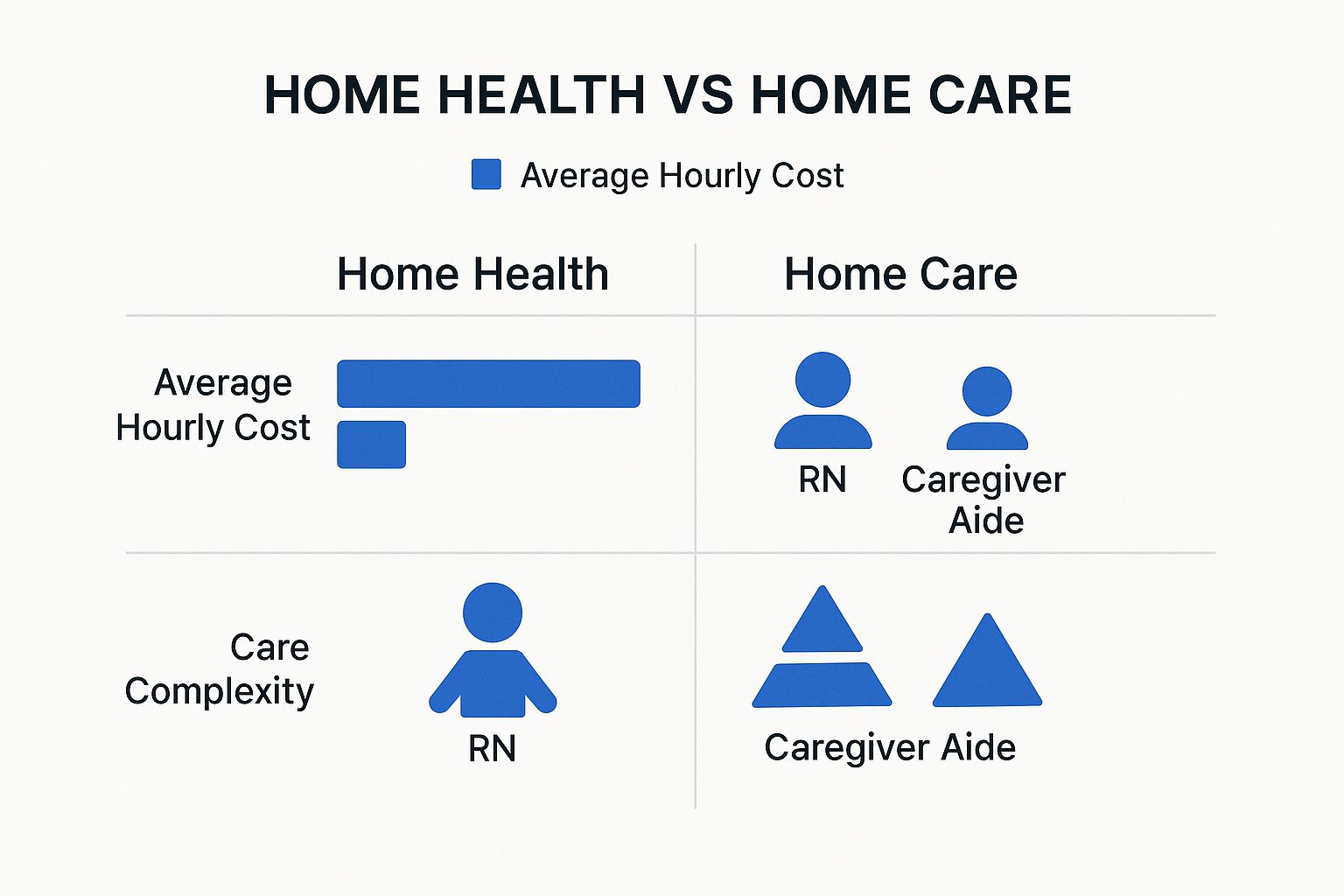
As you can see, the hourly costs for home health are higher. That’s because it involves professionals with advanced clinical training to handle more complex medical needs.
Home Health Vs Home Care Key Distinctions
To make the distinction even sharper, here’s a quick-reference table that puts the essential attributes of each service side-by-side.
| Attribute | Home Health Care | Home Care |
|---|---|---|
| Primary Goal | Treat a medical condition, help with recovery, or manage symptoms. | Provide personal assistance, companionship, and support for daily living. |
| Key Services | Skilled nursing, physical/occupational therapy, wound care, medication administration. | Bathing, dressing, meal prep, light housekeeping, transportation, companionship. |
| Provider Type | Licensed clinicians: RNs, LPNs, Physical Therapists, Occupational Therapists. | Caregivers, home care aides, Certified Nursing Assistants (CNAs). |
| Requirement | Must be prescribed by a doctor as part of a formal care plan. | Does not need a doctor's order; can be set up directly by the family. |
The growth in this field has been incredible. The global home healthcare market was valued at $369.3 billion in 2022 and is expected to hit $797.8 billion by 2032. With over 12,200 Medicare-certified agencies in the U.S. alone, it’s clear this is a vital part of our modern healthcare system.
A Look at the Day-to-Day: What In-Home Services Actually Involve
Definitions on a page are one thing, but seeing how these services play out in a real home environment is where the choice between home health and home care becomes crystal clear. The daily tasks are worlds apart, each shaped by a completely different goal—one is focused on medical recovery, the other on supporting daily life.
Home health care is clinical, plain and simple. It’s structured around a doctor’s plan of care, and a typical visit is a targeted medical service performed by a licensed professional, not a general helping hand around the house.
For instance, a physical therapist might come in to guide someone through specific exercises to build strength after a hip replacement. Every part of that visit is goal-oriented, documented, and a piece of a larger, temporary treatment plan designed to get them back on their feet.
A Focus On Medical And Therapeutic Goals
The services that fall under the home health umbrella are diverse, but they all share one thing in common: they are medical in nature. Each task requires specialized training, a license, or a certification to perform.
Here are a few common examples of what this looks like:
- Skilled Nursing: A registered nurse (RN) might be there to provide expert wound care for a surgical incision, manage a complex IV line, or spend time educating a patient on how to manage their new diabetes diagnosis.
- Physical Therapy (PT): You’ll see a therapist helping a stroke survivor relearn how to walk safely or using very specific exercises to restore mobility after an injury.
- Occupational Therapy (OT): An occupational therapist works hands-on with a client, helping them relearn the essential activities of daily living, like how to safely get dressed or prepare a simple meal.
The key takeaway for home health care is that it's designed to be temporary and rehabilitative. The main objective is to help the patient recover, become independent in managing their health, and, eventually, no longer need the services.
A Focus On Personal Support And Independence
Home care, on the other hand, is all about providing the practical, non-medical support that makes daily life at home safer, easier, and more enjoyable. These services are often needed long-term and are built to help people maintain their independence for as long as possible.
A home care aide’s day is built around the client’s personal routine and immediate needs. This could mean starting the morning by helping them get out of bed and dressed, then moving on to preparing a nutritious breakfast and giving a friendly medication reminder.
They also provide crucial help with what are known as Instrumental Activities of Daily Living (IADLs)—the more complex tasks we all need to manage to live independently. You can learn more about what are instrumental activities of daily living to get a fuller picture of this type of care. These activities frequently include:
- Meal preparation and grocery shopping
- Transportation to doctor’s appointments or social outings
- Light housekeeping and laundry
- Companionship and social interaction
Official resources, like this guide from Medicare.gov, make it clear that getting started with home health care is a formal medical process.

This screenshot really highlights a core difference: home health care always starts with a doctor's order and a formal evaluation. This is a stark contrast to the more flexible, needs-based approach of home care, which can be arranged directly by a family whenever support is needed.
Understanding Who Delivers the Care
The biggest difference between home health and home care really comes down to who walks through your door. The person you welcome into your home has a specific set of skills, qualifications, and legal credentials, and that’s what defines the kind of support they can give. Getting this right is crucial for ensuring your loved one is safe, receiving quality care, and that everyone is accountable.
Simply put, home health care is provided exclusively by licensed medical professionals. These are clinicians who have gone through formal education, passed state board exams, and must follow strict standards of practice to keep their licenses. Their work is all about clinical expertise and following a doctor-prescribed plan of care.
On the other hand, home care is handled by caregivers trained to help with personal needs and everyday activities. While many are Certified Nursing Assistants (CNAs), their main job is to provide support, not medical treatment.
The Licensed Clinicians of Home Health
When a home health agency sends someone to your home, you're getting a member of a coordinated medical team. These professionals aren't interchangeable; each one has a specialized, regulated role.
You’ll likely work with professionals like:
- Registered Nurses (RNs): They’re the ones managing the overall care plan, giving medications, handling complex wound care, and teaching patients and their families how to manage health conditions at home.
- Physical Therapists (PTs): These experts are all about restoring mobility and strength. They work with people recovering from an injury, illness, or surgery, guiding them through targeted exercises.
- Occupational Therapists (OTs): They focus on helping people regain the skills they need for daily living—things like bathing, dressing, and eating. They often bring in adaptive equipment and new techniques to make these tasks possible again.
A defining feature of home health is that every service is prescribed by a physician and performed by a state-licensed professional. This structure ensures a high level of clinical oversight and accountability for medical outcomes.

The Supportive Professionals of Home Care
Home care providers are the true backbone of long-term support at home. Their focus is on making daily life safer, more comfortable, and manageable. All their training centers on providing compassionate, hands-on assistance with personal tasks.
The main providers you’ll see are:
- Home Care Aides or Caregivers: These are the folks who help with Activities of Daily Living (ADLs) like bathing, grooming, and getting around the house safely.
- Certified Nursing Assistants (CNAs): A CNA has more formal training than a standard caregiver and can often handle more complex personal care tasks. However, they always work under a nurse’s supervision and are not permitted to perform skilled medical duties.
No matter which path you take, it’s absolutely essential to verify an agency’s credentials, insurance, and hiring standards. A reputable agency will always run thorough background checks and make sure their staff is properly trained and supervised. This gives you the peace of mind that your loved one is in safe, capable hands. Don’t skip this step—it’s a non-negotiable part of the process.
How to Navigate Costs and Payment Sources
Let's talk about one of the biggest pieces of the puzzle: the financial side. Figuring out how to pay for in-home support is a critical step, and the paths for home health and home care are completely different. One is treated as a medical necessity, while the other is a personal support service. Getting this right from the start can save you from a world of headaches and unexpected bills down the road.

When it comes to home health, you're almost always dealing with insurance. Why? Because these are medical treatments prescribed by a doctor to help someone recover from an illness, injury, or hospital stay. The costs get handled just like any other medical expense.
Home care, on the other hand, is seen as non-medical, long-term support. Because of that, it's typically paid for privately—or "out-of-pocket"—by the person receiving care or their family.
Covering Medically Necessary Home Health Care
Since home health is a prescribed medical service, there are well-established ways to pay for it. The most common route by far is Medicare, which can cover the full cost of eligible services for a limited period.
To get that Medicare coverage, a patient has to check a few specific boxes:
- Doctor's Orders: A physician must certify that the patient requires skilled nursing care or therapy.
- Homebound Status: The patient has to be certified as "homebound," which means it’s extremely difficult for them to leave home without help.
- Plan of Care: All services have to be part of a formal care plan that a doctor reviews on a regular basis.
Private health insurance and Medicaid are also in the mix, but the specific rules and coverage limits will vary depending on the plan and state. The goal of these policies is always the same: to fund short-term, targeted care that helps a patient get back on their feet.
The bottom line for home health funding is medical necessity. If the care is prescribed to treat a specific condition and helps the patient recover, insurance is designed to cover it.
It's also worth noting that the healthcare world is always changing, which can impact how these services are paid for. For instance, during the COVID-19 pandemic, there was a major drop in new home health care cases. This happened right as Medicare rolled out its Patient-Driven Groupings Model (PDGM), which shifted reimbursement from 60-day to 30-day episodes and prioritized clinical needs over the sheer volume of therapy provided.
Funding Options for Personal Home Care
Since home care is all about supporting daily living, not treating a medical condition, it usually isn't covered by standard health insurance or Medicare. This means families typically foot the bill directly.
However, that doesn't mean you're completely on your own. There are several other options that can help soften the financial blow. For a much deeper dive, you should check out our guide on the cost of home health care.
Here are the key funding sources to look into for home care:
- Long-Term Care Insurance: These policies are built specifically to cover long-term support and are a go-to funding source for many families.
- VA Benefits: Veterans may qualify for programs like Aid and Attendance, which can help pay for home care services.
- Medicaid Waivers: Some states have specific Medicaid waiver programs that provide funds for non-medical home care, helping people stay in their own homes instead of moving to a facility.
Thinking ahead about these costs is crucial, as they are often a long-term expense. Exploring these other funding streams early on can make all the difference in affording quality, consistent care.
Making the Right Choice for Your Specific Needs
Knowing the definitions of home health and home care is one thing, but applying that knowledge to a real-life situation is where it really counts. To make the decision-making process a little clearer, let's walk through a few common scenarios. Each one highlights a distinct need that points clearly toward one type of care—or sometimes, a combination of both.
These examples are designed to get you past the technical terms and help you assess what your loved one is actually going through. By seeing these services in action, you can feel more confident about picking the right support system for your family.
Scenario 1: Post-Surgery Recovery
Imagine your father, David, is coming home after a successful knee replacement. He’s motivated, but he can’t put any weight on his leg yet. He needs help managing his pain medication and requires daily attention to his surgical incision to keep it from getting infected. On top of that, his doctor has prescribed a specific set of exercises to get his mobility back.
- Primary Need: Skilled medical care to ensure he heals correctly and gets his strength back.
- Recommendation: This is a clear-cut case for home health care. A registered nurse can manage his wound care and medications, while a physical therapist visits a few times a week to guide him through his recovery exercises. This care is temporary, goal-oriented, and directly tied to his medical recovery.
When it comes to post-operative recovery, skilled clinical oversight isn't just a "nice-to-have"—it's a necessity. Home health provides the medical expertise needed to manage treatment plans, prevent complications, and get someone back on their feet safely.
Scenario 2: Living with Dementia
Now, think about Sarah, an elderly woman living with moderate dementia. Physically, she's healthy, but her cognitive decline makes it hard for her to remember to eat, manage her personal hygiene, and stay engaged. She gets lonely and sometimes wanders if left unsupervised, which is a major safety risk.
- Primary Need: Consistent, non-medical support for daily activities, safety, and companionship.
- Recommendation: Home care is the perfect fit here. A caregiver can visit daily to prepare meals, help with bathing and dressing, provide medication reminders, and offer that all-important companionship. Their presence ensures Sarah is safe, comfortable, and socially stimulated, which allows her to keep living in the familiar comfort of her own home.
The demand for this kind of support is only growing. With about 75% of adults over 50 saying they want to age in their own homes, the home care industry is projected to top $107 billion in revenue by 2025. You can explore more about these industry trends to see how the world of in-home support is changing.
Scenario 3: Managing a Chronic Illness
Finally, let’s look at Robert, who is managing a chronic condition like congestive heart failure (CHF). His doctor needs a nurse to check his vitals, handle his complex medication schedule, and teach him about his diet and fluid restrictions. But Robert also deals with weakness and fatigue that make it tough to cook, clean, or even get to his appointments.
- Primary Need: A mix of both clinical supervision and help with daily living.
- Recommendation: This situation calls for both home health and home care. A home health nurse can visit weekly to check his vitals and make sure his medical plan is on track. At the same time, a home care aide can come in several times a week to help with meals, light housekeeping, and transportation, taking care of all his non-medical needs.
Common Questions About In-Home Care
When you start looking into in-home support, a lot of practical questions naturally come up. Getting clear answers is the first step to coordinating care that actually works, finding providers you can trust, and making sure your loved one gets the right kind of help.
One of the first things families ask is whether someone can get both home health and home care at the same time. The answer is a definite yes—and honestly, it's often the best approach. The two services are designed to work together, not against each other, covering different but equally vital needs.
Think about someone recovering from a stroke. They might have a home health nurse visit weekly to check on medications and a physical therapist to rebuild mobility. At the same time, a home care aide could be there every day to help with meals, bathing, and just moving safely around the house. This kind of tag-team approach ensures that both the clinical and daily living needs are completely covered.
How Do You Find a Reputable Agency?
Finding an agency you feel good about is absolutely critical for your peace of mind. Vetting providers doesn't have to be a huge headache if you just follow a few key steps to check for quality and safety.
Start by making a shortlist of local agencies. A fantastic place to begin is Medicare's official Care Compare tool. It lets you find and compare certified agencies using real patient survey results and quality ratings.
From there, it's all about verifying their credentials. Always make sure the agency:
- Holds a current state license to operate.
- Is bonded and insured, which protects you from any liability.
- Runs thorough background checks on every single employee.
- Provides its staff with ongoing training and supervision.
A great way to gauge an agency's commitment to quality is to ask directly about their hiring process and training programs. A provider who takes pride in their work will be happy to tell you all about it.
What Is the Difference Between a Home Health Aide and a Caregiver?
While people sometimes use these terms interchangeably, the roles are quite different, and so is the training. A home health aide (HHA) has gone through formal medical training and certification. This allows them to handle specific clinical tasks under a nurse's direction, like taking vital signs or assisting with prescribed therapies.
A caregiver, often called a home care aide, is trained to provide non-medical, personal support. Their expertise is in helping with activities of daily living—things like meal prep, bathing, and companionship—to ensure a safe and comfortable home environment. Knowing this difference is the key to matching the right professional to what your family truly needs.
At NJ Caregiving, we specialize in providing compassionate and professional in-home care services tailored to your specific situation. Learn more about how our dedicated team can support your family's journey by visiting https://njcaregiving.com.


