When a family member needs constant medical attention, figuring out the best path forward can feel overwhelming. That's where 24 hour in home nursing comes in. At its heart, this service provides round-the-clock medical care from licensed professionals, all within the familiar, comforting walls of a patient's own home.
Think of it as bringing the skilled, watchful eye of a hospital-level care team directly to you.
What 24 Hour In Home Nursing Truly Means
This level of support is far more than just having someone around for companionship. It’s a clinical service built for individuals with complex medical needs who require constant monitoring and skilled, professional help. It beautifully bridges the gap between a hospital stay and safely returning home, ensuring no detail is missed.
The demand for this kind of care is growing fast. As of 2025, the home nursing care market spans 195 countries, a number that keeps climbing thanks to aging populations and a rise in chronic conditions. It's a clear sign that families value keeping their loved ones at home whenever possible.
Unlike standard home care, 24-hour nursing is delivered by a team of licensed professionals. Each person has a specific role, all working together to follow a doctor's plan of care and make sure every medical need is met with precision.
The chart below shows how these professionals typically work together to provide comprehensive care.
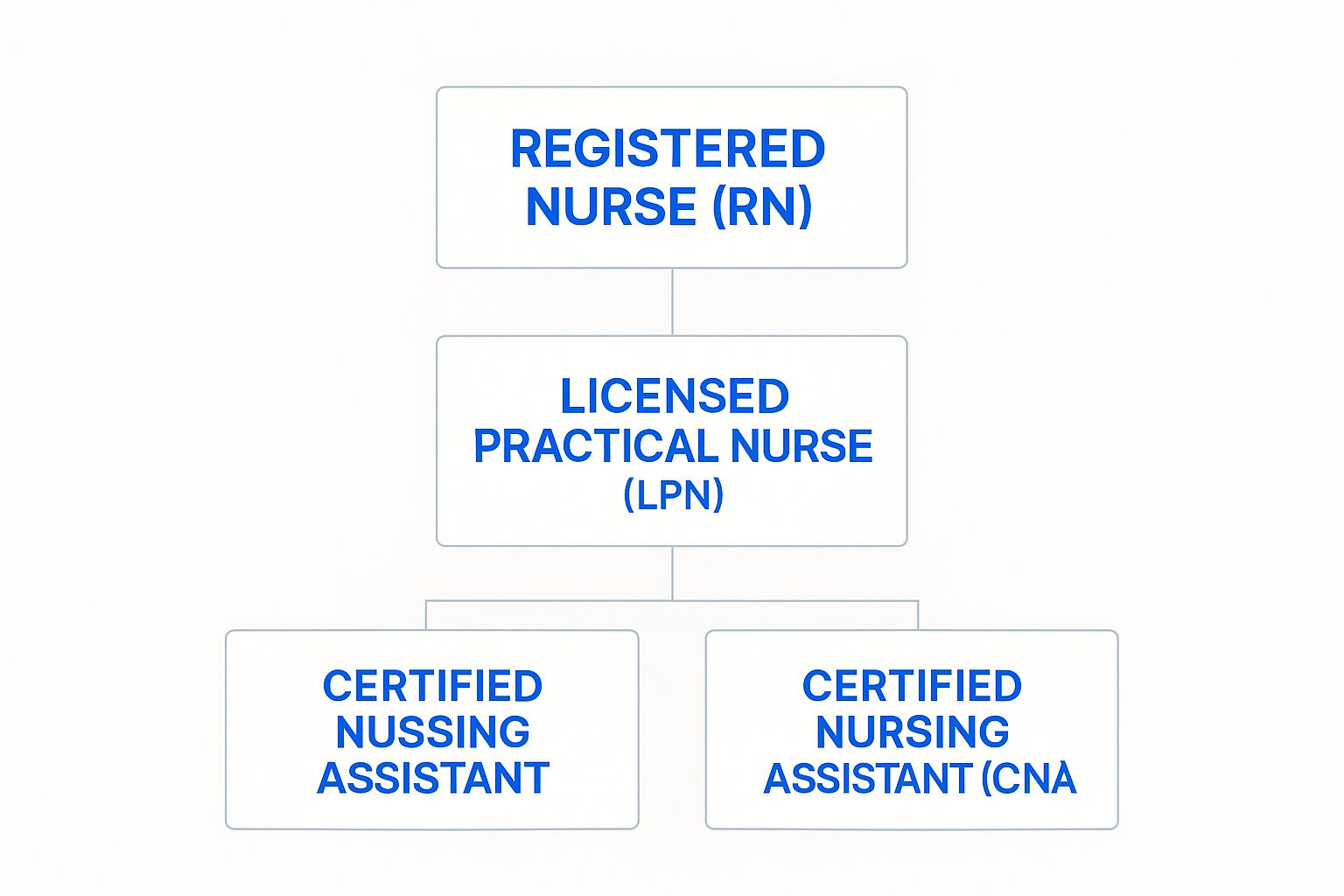
This team structure ensures every task is handled by the right person, from a Registered Nurse managing the overall care plan to a Certified Nursing Assistant helping with daily activities.
Two Primary Models of Care Delivery
To provide this continuous coverage, agencies generally use one of two main approaches. Understanding the difference is the first step in finding the right fit for your family's situation.
To help you see the differences at a glance, here’s a quick comparison of the two main ways 24-hour care is structured.
Comparing 24 Hour Care Models
| Feature | Shift-Based Care | Live-In Care |
|---|---|---|
| Staffing | A team of 2-3 nurses works in 8-12 hour shifts | One primary caregiver resides in the home for several days |
| Cost | Typically higher due to multiple caregivers | More cost-effective as it involves fewer staff members |
| Caregiver State | Always fresh, alert, and focused on the patient | Caregiver requires a private room and designated sleep breaks |
| Best For | Patients with intensive, complex, or unpredictable needs | Patients who are stable but need a professional presence |
Ultimately, both models are designed to create a seamless safety net. They prevent dangerous gaps in care that might otherwise lead to a health crisis or a trip back to the hospital.
- Shift-Based Care: This model involves multiple nurses—usually two or three—working in 8 to 12-hour shifts. This ensures there is always a fresh, alert, and focused professional on duty, which is perfect for patients with highly intensive or unpredictable needs. It’s the most robust and vigilant form of medical supervision you can get at home.
- Live-In Care: With this setup, a single nurse lives in the home for a few days at a time. This arrangement requires giving the caregiver a private space to sleep and take designated breaks. It’s often a great fit for patients who are stable but still need a professional nearby for safety and periodic medical tasks.
The goal of both models is to provide a seamless safety net, preventing gaps in care that could lead to hospital readmissions or health complications. This continuity is the cornerstone of effective 24-hour nursing.
Choosing between them really comes down to the specific medical needs of your loved one and what feels right for your family. If you'd like to see what this dedicated care looks like in action, you can view our photo gallery of our care professionals.
When Is Round-The-Clock Nursing Care Necessary?

It can be tough for families to recognize the exact moment when a little extra help at home just isn't enough anymore. The line between needing some assistance and requiring constant, skilled medical supervision can blur, sometimes shifting gradually and other times changing in an instant.
Knowing the specific signs that point to a need for 24-hour in-home nursing is key. It helps you advocate for the right level of care when it matters most.
Think of it this way: companion care is like having a kind, helpful neighbor pop in, while 24-hour nursing is like having a dedicated medical professional living right there with you. It becomes the right choice when a loved one's health demands more than an extra pair of hands—it requires the constant presence of a licensed professional who can make clinical judgments on the spot.
This shift often happens when managing complex medical needs becomes an around-the-clock job, one that goes far beyond simple reminders or basic help.
Situations Demanding Continuous Medical Oversight
Some health journeys simply require a level of watchfulness that only a professional nurse can provide. These situations usually involve unstable conditions, complicated treatments, or a high risk of sudden problems.
A common trigger is the recovery period after a major surgery, like a heart bypass or joint replacement. Those first few weeks back at home are a critical window for monitoring vital signs, managing prescription pain medication, and watching for any signs of infection. A skilled nurse provides the professional oversight needed to get through this fragile period safely.
Progressive neurological conditions are another area where this level of care becomes essential.
- Advanced Dementia or Alzheimer's: In the later stages, severe cognitive decline can make it unsafe for a person to be alone. They might wander, forget to eat, or be unable to communicate urgent medical symptoms. Constant supervision becomes necessary.
- ALS (Lou Gehrig's Disease): As the disease progresses, many patients rely on medical equipment like feeding tubes or ventilators to breathe. This is sophisticated technology that requires a licensed nurse to operate and troubleshoot, ensuring that life support is always functioning correctly.
End-of-Life and Palliative Care Needs
Helping a loved one stay comfortable and maintain their dignity during the final stages of life is a profound act of love, but it often requires professional medical support. While hospice services are wonderful for managing pain and improving quality of life, they typically don't include continuous, 24-hour care unless a short-term crisis pops up. This is a critical gap that 24-hour in-home nursing is designed to fill.
For someone receiving palliative care at home, a dedicated nurse ensures that symptoms like severe pain or breathing difficulties are managed immediately, no matter the time of day or night. This constant presence provides incredible peace of mind to both the patient and their family.
The goal is to create an environment where the patient is comfortable, their symptoms are controlled, and the family can focus on spending meaningful time together rather than worrying about medical crises.
Ultimately, the decision to bring in round-the-clock nursing is about ensuring safety and providing the highest quality of life possible. It’s the right call when a loved one's medical needs have grown beyond what family members can safely manage on their own. Recognizing these signs empowers you to give them the compassionate, professional care they truly deserve.
Breaking Down the Cost of 24 Hour Home Nursing
For most families, the financial side of 24 hour in home nursing is naturally the biggest question. The cost can feel intimidating at first, but once you understand what goes into it, planning and budgeting become much more manageable. The final price isn't just a single number—it's a reflection of several key factors working together.
Think of it like building a custom home. You have a base price for the structure, but the final cost depends on the specific materials, the location, and any unique features you add. In the same way, the price of around-the-clock nursing is shaped by your loved one's specific medical needs and where you live.
This is an investment in having a licensed professional always present to manage complex medical needs, providing a level of safety and expertise that is truly priceless.
Core Factors That Influence the Price
A few key variables directly impact the daily or monthly cost of care. The most significant one is the level of medical complexity involved. A patient recovering from surgery who needs wound care and medication management will have different cost factors than someone who requires ventilator support or ongoing intravenous therapies.
Another major driver is your geographic location. Just like the cost of living varies from state to state, so do the rates for skilled nursing professionals. Densely populated urban areas often have higher agency rates than rural communities due to higher operational costs and a greater demand for qualified nurses.
The national monthly average for 24-hour in-home nursing care is approximately $18,144 in 2025, with a typical range falling between $15,000 and $25,000. Hourly rates average around $27, but this can climb higher in major metropolitan areas with a higher cost of living. Learn more about the factors driving these costs.
This data gives you a solid baseline, but remember, your specific quote will always depend on a personalized assessment of your family's needs.
Shift-Based vs. Live-In Pricing Models
The type of care model you choose also plays a crucial role in the overall cost. As we’ve touched on, shift-based and live-in care are structured differently, and that’s reflected in their pricing.
- Shift-Based Care: This is often the more expensive option because it involves paying the full hourly rate for two or three nurses to cover a 24-hour period. You're paying for constant, active coverage without breaks, ensuring a fresh and alert caregiver is always on duty. This model is essential for patients with acute or unpredictable needs.
- Live-In Care: This model is typically more cost-effective. Instead of an hourly rate for all 24 hours, you usually pay a flat daily rate. This is because the caregiver is provided with room, board, and mandated rest periods. It’s an excellent option for stable patients who need the security of a professional presence but don't require intensive, minute-to-minute medical care around the clock.
Looking Beyond the Hourly Rate
When you’re budgeting, it’s important to think about potential costs that go beyond the nurse's time. A good agency will be transparent about these from the start, but it’s always smart to ask.
These additional expenses might include:
- Agency Administrative Fees: These cover the background work like caregiver screening, insurance, scheduling, and clinical oversight.
- Medical Supplies: While some supplies may be covered by insurance, you might need to budget for others, like specialized wound dressings or nutritional supplements.
- Holiday Pay: Most agencies charge a higher rate (often time-and-a-half) for services provided on major holidays.
Understanding all these elements gives you the complete financial picture, so there are no surprises down the road. It allows you to plan with confidence. At NJ Caregiving, we pride ourselves on providing clear, upfront pricing, which you can see in our detailed service guides. By knowing what to expect, you can focus on what truly matters: your loved one’s health and well-being.
Finding Ways to Fund In Home Nursing Care

Once you understand the costs that come with 24-hour in-home nursing, the next big step is figuring out how to actually pay for it. For many families, this is where the real work begins.
Diving into the world of healthcare funding can feel like learning a whole new language. It’s full of specific rules, confusing jargon, and strict requirements. But don’t worry—with a clear roadmap, you can confidently sort through the financial resources available to your family. This is about building a sustainable plan that ensures your loved one gets the uninterrupted, high-quality care they deserve.
Let’s break down the most common funding avenues, one by one.
The Role of Medicare and Medicaid
It's natural for families to look toward government programs first, but it’s so important to know what they will and won't cover when it comes to continuous nursing care.
Medicare is a big one, but it generally does not cover long-term, 24-hour care at home. Think of Medicare as a short-term solution. It’s designed for intermittent care right after a hospital stay or to address specific, temporary medical needs, not for around-the-clock supervision.
Medicaid, on the other hand, can be a huge help for long-term care, including in-home nursing. The catch? Eligibility is tied to very strict income and asset limits that vary by state. Medicaid services are often available through "waiver" programs specifically designed to help people stay in their own homes instead of moving to a nursing facility.
Private Insurance and Veterans Benefits
Beyond the big government programs, a few other key options can provide some serious financial support.
If your loved one was proactive and has Long-Term Care Insurance, now is the time to pull out that policy. This type of insurance is designed specifically to cover services like in-home nursing. Be sure to review the details closely.
- Benefit Triggers: What exactly has to happen for the policy to start paying? Usually, it's an inability to perform a certain number of daily living activities.
- Daily/Monthly Limits: Find out the maximum amount the policy will pay out each day or month. This is a critical number for budgeting.
- Elimination Period: This is basically a waiting period—think of it like a deductible—before the benefits kick in.
For those who have served our country, Veterans Affairs (VA) benefits can be another lifeline. The VA offers several programs, like Aid and Attendance, which can provide a monthly pension to help cover the costs of in-home care for qualified veterans and their spouses.
Comparing Your Funding Options
Every funding source has its own rulebook and works best in different scenarios. Seeing them all side-by-side can make it much clearer which path your family should explore first.
Here's a quick look at how the main funding sources stack up for paying for round-the-clock care.
Funding Sources for In-Home Nursing Care
| Funding Source | Typical Coverage for 24-Hour Care | Key Eligibility Criteria | Best For |
|---|---|---|---|
| Medicare | Very limited; typically only short-term or during an acute crisis | Must be "homebound" and require skilled, intermittent care | Post-hospitalization recovery or specific, doctor-ordered treatments |
| Medicaid | Can be comprehensive through state waiver programs | Strict income and asset limitations set by the state | Low-income individuals with significant, long-term medical needs |
| Long-Term Care Insurance | Often covers a significant portion, based on policy limits | Must meet the policy's benefit triggers (e.g., inability to perform ADLs) | Individuals who planned ahead and purchased a private policy |
| Veterans Benefits | Can provide a monthly pension to help offset costs | Must meet specific service, disability, and financial requirements | Eligible veterans, their spouses, or surviving spouses |
| Private Pay | Full coverage, paid directly by the family | N/A | Families with the financial means or those bridging gaps in insurance |
Don't feel like you have to pick just one. Many families find success by combining multiple sources—like using a long-term care policy and then covering the rest with private funds—to create a complete financial solution.
Securing funding for 24-hour in-home nursing takes a bit of work. It requires research, persistence, and a close eye on the details. But by understanding all the options on the table, you can piece together the resources needed to give your loved one the best care possible, right in the comfort of their own home.
How to Find a Trusted Home Nursing Provider
Choosing an agency for 24 hour in home nursing is one of the most critical decisions you'll ever make. This isn't just about hiring a service; it’s about inviting a professional into your home and entrusting them with a loved one's well-being. Thinking about it systematically can turn what feels like a daunting task into a confident choice.
It helps to think of this as hiring a key member of your family’s team. You wouldn’t bring someone in without checking their qualifications, asking the tough questions, and making sure they're a good fit. The same exact principles apply here to make sure you find a provider who delivers both top-tier clinical skill and genuine, compassionate support.
The good news is that the demand for skilled in-home professionals has created a strong and growing workforce. Between 2014 and 2023, the number of direct care workers in the U.S. shot up from 3.5 million to 5 million, and there are nearly 4.7 million registered nurses nationwide. You can find more insights about the growth in home health services to see just how much the options have expanded. This growth means you have more choices, which makes a thorough vetting process more important than ever.
Verifying Credentials and Accreditations
Your first move should be to create a shortlist of agencies and then confirm they meet all the essential professional standards. This isn't just about checking boxes; it’s about safety and quality. Any reputable provider will be completely transparent and proud of their credentials.
Start by checking for a state license. Every state has its own set of rules for home health agencies, and a license proves the agency is legally allowed to operate. Next, look for accreditations from national organizations like The Joint Commission or the Community Health Accreditation Partner (CHAP). These aren't easy to get, and they signal a real commitment to the highest standards of care.
A licensed and accredited agency demonstrates a commitment to patient safety and quality that goes far beyond the bare minimum. It’s a clear indicator that they adhere to rigorous, nationally recognized standards of care.
Key Questions to Ask During Consultations
Once you have a list of qualified agencies, it's time to start the interviews. A consultation is your chance to really dig in, and their answers will tell you a lot about their operational standards and care philosophy. Don't be shy about asking detailed questions—the right agency will appreciate your diligence.
It’s a good idea to prepare a list of questions that covers everything from caregiver qualifications to what happens in an emergency. This helps you gather the same information from each provider, making it much easier to compare them side-by-side later.
Here are a few essential questions you absolutely must ask:
- Caregiver Screening: "What is your screening process for new nurses and caregivers? Does it include comprehensive background checks, license verification, and reference checks?"
- Staff Training: "What kind of ongoing training do your nurses receive? Do they have specialized training for conditions like dementia or managing a ventilator?"
- Emergency Protocols: "What is your procedure if a medical emergency happens? How do you ensure a backup nurse is available if our primary caregiver is sick or delayed?"
- Supervision: "How is the in-home nursing staff supervised? Will a clinical supervisor or Director of Nursing make regular visits to oversee the plan of care?"
These kinds of questions help you see past the marketing brochures and understand how an agency truly operates day-to-day. We outline our own commitment to quality and transparency in our caregiving service details.
Reviewing Contracts and Gauging Compatibility
Before you sign on the dotted line, carefully review the service agreement or contract. Pay close attention to the fine print on rates, payment schedules, cancellation policies, and exactly what services are included. A clear, easy-to-understand contract is the mark of a professional organization.
Finally, trust your gut. The relationship between a nurse, the patient, and the family is deeply personal. As you talk with potential agencies, try to get a feel for their communication style. Do they actually listen to your concerns? Are they compassionate and respectful? Finding a provider that aligns with your family’s values is every bit as important as finding one with impeccable credentials.
Common Questions About 24-Hour Nursing Care

Exploring the world of 24-hour in-home nursing naturally brings up a lot of questions. As you think about this big step for your family, getting clear, direct answers is the best way to move forward with confidence.
This is about more than just logistics—it’s about finding peace of mind. By tackling the most common concerns head-on, you can get a much clearer picture of how this level of care actually works inside a home.
Below, we’ve answered the key questions we hear most often from families just like yours.
What Is The Difference Between 24-Hour Home Care and 24-Hour In-Home Nursing?
This is probably the most critical distinction to get right, because these two services solve very different problems. The main difference is the medical skill and licensing of the person providing the support.
Think of it as the difference between a helpful friend and a registered nurse. Both are incredibly valuable, but you’d call them for completely different reasons.
- 24-Hour Home Care: This is handled by non-medical caregivers or home health aides. They provide essential help with activities of daily living (ADLs)—things like bathing, dressing, making meals, and companionship. Their job is to offer supervision and personal assistance, but they are not licensed to perform medical tasks.
- 24-Hour In-Home Nursing: This is a clinical service provided by licensed nurses, like a Registered Nurse (RN) or a Licensed Practical Nurse (LPN). These are trained professionals who can administer medication, manage complex equipment like ventilators, handle wound care, and execute a doctor's detailed care plan.
The bottom line is medical capability. If your loved one mainly needs supervision and personal support, home care is the right fit. But if they need ongoing medical treatment and monitoring, you absolutely need 24-hour in-home nursing.
How Do Live-In Nurses Get Enough Rest To Provide Safe Care?
This is an excellent and very important question. A tired caregiver simply can't provide safe care, and any good agency has strict rules to prevent burnout and make sure every nurse is sharp and ready to help.
A live-in nurse isn’t expected to be awake and on duty for 24 hours straight. By law, they must be given a private place to sleep and an uninterrupted rest period of at least 8 hours. They also get meal breaks throughout their day.
The safety of both the patient and the caregiver is the top priority. If a patient's condition is unstable and they're likely to need help frequently during the night, a responsible agency will recommend using multiple nurses working in shifts instead of a single live-in nurse.
This ensures there’s always a fresh, rested professional on hand to respond to any need that comes up. Before you sign with any agency, always ask about their specific policies on caregiver rest, breaks, and what their protocol is if the patient’s needs interrupt that designated sleep time.
Can Our Family Supplement Care To Reduce Nursing Hours?
Absolutely. In fact, many families create a hybrid care plan to manage costs while ensuring their loved one gets all the support they need. This team approach can be a wonderfully practical and sustainable solution.
For instance, a family might hire a professional nurse for 16 hours a day to cover the most medically intensive periods, like daytime medication schedules and overnight monitoring. Then, a trained and capable family member could step in to cover the remaining 8-hour shift.
This kind of arrangement works best when:
- The patient's condition is relatively stable during the hours the family is covering.
- The family caregiver feels confident and is properly trained to handle the patient’s needs.
- No complex medical tasks are required during the family-covered shift.
Open and honest communication with the nursing agency is the key here. A great provider will work with you to create a safe, coordinated plan that smoothly blends professional support with family involvement, respecting both your budget and your loved one’s well-being.
What Happens If We Are Not Compatible With The Assigned Nurse?
Personal chemistry is such a vital piece of the puzzle. The connection between a nurse, the patient, and the family can make or break the entire experience, so it’s crucial that everyone feels comfortable.
A high-quality home nursing agency gets this. They should have a clear and supportive process for handling compatibility issues. Remember, you’re not just hiring a set of clinical skills; you’re inviting a person into the private space of your home.
If the first nurse assigned isn't the right fit for your loved one’s personality or your family’s dynamic, you should feel completely empowered to ask for a change. It's a normal and very reasonable request.
Before signing a contract, make sure you ask the agency about two specific things:
- Their Matching Process: How do they choose a nurse for a new client in the first place? Do they take personality, communication style, and experience with certain conditions into account?
- Their Reassignment Policy: What’s the exact process if you need to request a different nurse? How quickly can they make that happen?
A trustworthy provider will make finding the right match a priority. They will work with you to ensure a comfortable, trusting, and supportive environment is established right from the start.



