When we talk about caring for a loved one, you'll often hear the term Activities of Daily Living, or ADLs. These are simply the essential self-care tasks we all do every day to take care of our basic physical needs. Think of them as the fundamental skills for living on your own—everything from getting out of bed in the morning to getting ready for sleep at night.
Understanding the Building Blocks of Independence

When we ask, "what are activities of daily living," we're really digging into the core functions that allow someone to live safely and independently. These are the daily routines so ingrained in our lives that we barely notice them. That is, until an illness, an injury, or simply the natural process of aging makes them a real challenge.
The concept of ADLs has become a cornerstone in healthcare, particularly in senior care. It gives families and medical professionals a practical framework to gauge a person's abilities and figure out the right level of support they might need.
The Two Main Categories of ADLs
To get a clearer picture of a person's independence, experts break these tasks into two distinct groups. This separation helps paint a more complete picture of someone's strengths and where they might be struggling.
- Basic Activities of Daily Living (BADLs): These are the most fundamental self-care tasks tied to personal hygiene and getting around. They answer the basic question, "Can this person take care of their own body?"
- Instrumental Activities of Daily Living (IADLs): These are the more complex activities needed to manage a household and live independently in the community. They address the question, "Can this person manage their home and interact with the world around them?"
For now, this guide will focus on the six core BADLs, as they are the most critical signals that someone may need hands-on care.
As our loved ones age, it may become more difficult for them to perform these daily activities. Understanding what ADLs are can help you determine how much care and assistance your loved ones need.
The growing need for help in these areas is easy to see in the demand for assistive tools. The global market for devices related to ADLs was valued at around $15 billion in 2025 and is expected to climb, potentially hitting $25 billion by 2033. This surge shows just how much focus is being placed on finding solutions to help people hold onto their independence. You can find out more about the ADL devices market trends and research.
To help break it down, here’s a quick overview of the main activities that define a person's ability to care for themselves.
Core Activities of Daily Living at a Glance
This table summarizes the six essential ADLs that form the foundation of personal self-care. It outlines what each activity involves in a practical sense.
| Activity of Daily Living | What It Involves |
|---|---|
| Eating | The ability to feed oneself, which includes getting food from a plate into the mouth. |
| Bathing and Hygiene | The capacity to wash one's face and body in a bath or shower and perform grooming like shaving or brushing teeth. |
| Dressing | The skill of choosing appropriate clothes and putting them on, including handling zippers, buttons, and shoes. |
| Toileting | Being able to get to and from the toilet, use it correctly, and clean oneself afterward. |
| Mobility (Ambulating) | The ability to move from a bed or chair and walk from one place to another without assistance. |
| Continence | Having full and voluntary control over bladder and bowel functions. |
Keeping these six activities in mind provides a clear and simple checklist when you're trying to assess a loved one's needs.
Basic ADLs vs. Instrumental ADLs
When we talk about "activities of daily living," it's easy to lump everything together. But to truly understand a person's ability to live independently, we need to break it down into two distinct categories. Think of it like building a house. You have to pour a solid foundation before you can even think about putting up the walls, windows, and roof.
The same idea applies here. The two main types are Basic Activities of Daily Living (BADLs) and Instrumental Activities of Daily Living (IADLs). While the names sound similar, the difference between them is huge. Spotting these differences is often the very first step in recognizing that a loved one might need a bit more support.
Understanding Basic ADLs
Basic ADLs, often just called ADLs, are the absolute building blocks of self-care. These are the fundamental tasks we all need to do to take care of our own bodies. They're the non-negotiable things we do every day, usually without giving them a second thought.
The six core BADLs are all about personal survival and include skills like:
- Eating (the ability to feed oneself)
- Bathing and keeping up with personal hygiene
- Dressing and choosing the right clothes for the day
- Toileting (getting to the toilet and using it independently)
- Mobility (being able to move, walk, and transfer from a bed to a chair)
- Continence (maintaining control over bladder and bowels)
When someone starts to struggle with these tasks, it's a clear sign they may need more direct, hands-on help.
Grasping Instrumental ADLs
Instrumental ADLs are the next step up in personal independence. While they aren't strictly essential for basic survival, they are the skills we need to manage a household and live safely within our community. Think of these as requiring more complex planning and organization.
The simplest way to put it is that BADLs are about caring for your body, while IADLs are about caring for your life. A person can be perfectly capable of all their BADLs but still struggle to live alone if they can't manage their IADLs.
This is often where families first notice subtle changes. Common IADLs include things like managing money, preparing meals, shopping for necessities, and navigating transportation.
This image highlights just how many more tasks fall under the IADL category, painting a broader picture of what it takes to live independently.
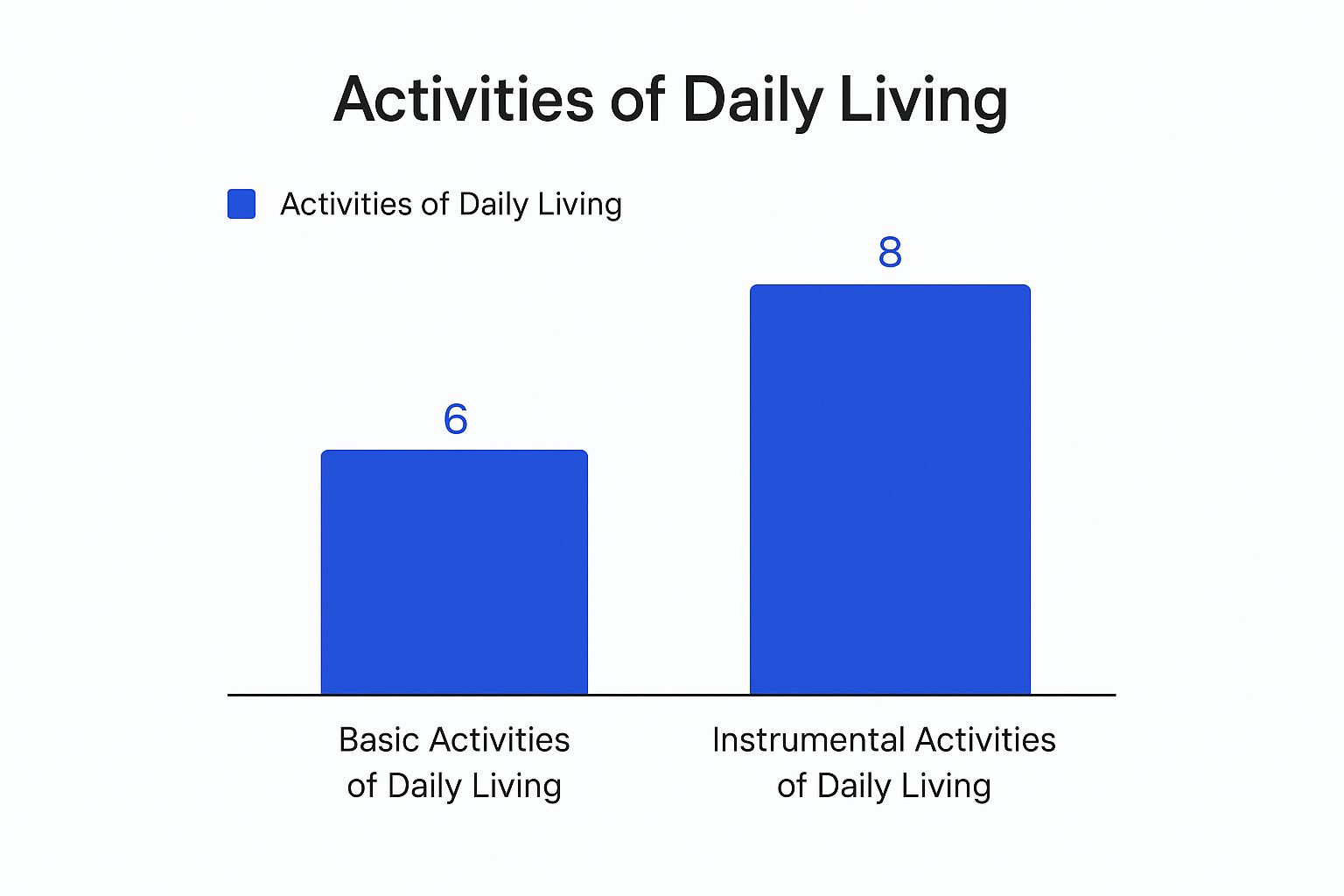
As you can see, IADLs cover a much wider range of complex life-management skills compared to the essential self-care focus of BADLs.
To make the distinction even clearer, let's look at them side-by-side.
Comparing Basic ADLs vs. Instrumental ADLs
This table provides a simple comparison of Basic and Instrumental ADLs, showing their key differences and giving concrete examples for each.
| Aspect | Basic Activities of Daily Living (BADLs) | Instrumental Activities of Daily Living (IADLs) |
|---|---|---|
| Main Focus | Core self-care tasks for personal survival and hygiene. | More complex skills needed to live independently in the community. |
| Examples | Bathing, dressing, eating, getting around the house. | Cooking, managing money, shopping, using the phone, cleaning. |
| Cognitive Skill Level | Requires less complex cognitive function. | Requires higher-level planning, organization, and problem-solving. |
| Typical Timing of Decline | Difficulties often appear in later stages of decline. | Challenges often surface as early warning signs of needing support. |
This breakdown helps clarify why both categories are so important for assessing a person's true needs.
Why This Distinction Matters for Care Planning
Separating these two types of activities is critical because problems with IADLs almost always show up before challenges with BADLs. For example, a parent might start forgetting to pay bills or let fresh groceries go bad long before they have any trouble getting dressed in the morning.
These early IADL struggles are crucial warning signs.
This progression gives families a window of opportunity to be proactive. When you spot IADL difficulties early, you can arrange for support—like a meal delivery service, transportation help, or assistance with finances—before a more serious health or safety crisis happens.
Understanding this difference allows families and healthcare providers to develop a much more precise and effective care plan. It ensures that support is introduced at the right time and targets the specific needs of the individual, preserving their dignity and maximizing their independence for as long as possible.
Why ADLs Are So Important in Senior Care and Healthcare

Understanding Activities of Daily Living is about more than learning a new piece of jargon. It’s about grasping a core concept that serves as the very foundation for how we approach senior care and healthcare today. An ADL assessment isn’t a test someone passes or fails. It's a powerful tool that gives us a clear, honest picture of a person’s ability to live independently.
Think of an ADL evaluation as a roadmap for care. It helps doctors, therapists, family members, and care providers like NJ Caregiving see exactly where a person is on their health journey. This insight is what allows us to make informed, compassionate decisions that protect an individual's safety, dignity, and quality of life. Without this framework, planning for care feels a lot like trying to find your way in the dark.
Shaping Truly Personal Care Plans
One of the most powerful uses for an ADL assessment is building a care plan that is genuinely personalized. A one-size-fits-all approach just doesn't cut it when you’re supporting a person with their own unique set of strengths and challenges. By pinpointing the specific ADLs that are becoming difficult, a care plan can deliver the right kind of help at precisely the right time.
For example, if your dad can still dress himself and eat without issue but struggles to get in and out of the shower safely, the care plan can focus specifically on bathing assistance. This targeted support avoids unnecessary intrusion, empowering him to maintain control over the parts of his life he can still manage on his own. It’s an approach built on respect and autonomy.
This is more important than ever, as challenges with daily tasks are incredibly common. Globally, nearly half of all people over 60 face difficulties with everyday activities. Conditions like Alzheimer's, which affects both cognitive and physical abilities, have a huge impact on a person's ability to handle ADLs. In 2025, an estimated 7.2 million Americans aged 65 and older will be living with this disease—a figure projected to nearly double by 2050. Discover more insights about the impact of Alzheimer's on daily living.
Determining Who Qualifies for Support and Services
Beyond creating a day-to-day care plan, a person's ADL status is the key that unlocks eligibility for many essential support services. It acts as a standardized yardstick that insurance companies and government programs use to measure a person's level of need.
An ADL assessment provides the objective evidence needed to access vital resources. It shifts the conversation from, "I think Mom needs help," to, "Mom is unable to perform two of the six basic ADLs, which qualifies her for support."
This is especially critical for programs and policies like:
- Long-Term Care Insurance: Most policies have benefit triggers tied directly to being unable to perform a certain number of ADLs, usually two or three. A formal assessment gives you the documentation needed to activate those benefits.
- Medicaid Home and Community-Based Services: To qualify for programs that help seniors age safely at home, you often have to demonstrate a need for assistance with ADLs.
- Medicare Coverage: In some cases, Medicare will cover home health services or essential medical equipment, but only if it's proven necessary for managing ADLs at home.
For families here in Mercer County, understanding how these assessments work is the first step toward getting the financial and practical support required for quality in-home care.
Guiding Decisions About Living Arrangements and Safety
Finally, having a clear picture of someone’s ADL capabilities is absolutely essential when making big decisions about their living environment. The number one goal is always to keep them safe while helping them be as independent as possible.
An ADL evaluation helps you answer those tough but necessary questions:
- Is it still safe for my parent to live alone?
- Would a few hours of in-home care each day be enough?
- Is it time to consider the more comprehensive support of an assisted living community?
If someone only needs a hand with IADLs like cooking or getting to appointments, in-home care can be the perfect fit to help them stay in their own home. But if they start having trouble with basic ADLs like walking or using the toilet, a higher level of care might be needed to prevent falls and other serious risks.
Ultimately, by zeroing in on the Activities of Daily Living, we put the focus right where it belongs: on preserving dignity, ensuring safety, and providing the exact support someone needs to live a full and meaningful life.
How Professionals Assess Activities of Daily Living
When you start to notice a loved one struggling with everyday tasks, the thought of a "formal assessment" can sound pretty intimidating. But it’s not about passing or failing a test.
Think of it as creating a clear, objective snapshot of where they are right now. This process gives everyone—doctors, caregivers, and family—a consistent way to measure independence, track changes over time, and make sure the care plan is a perfect fit. Instead of guessing, these structured evaluations build a reliable picture of their abilities.
The Standardized Tools of Assessment
To get an accurate picture, healthcare providers like doctors, nurses, and occupational therapists use established assessment scales. These are essentially guided conversations or checklists that ensure nothing gets missed. Two of the most common tools you'll hear about are the Katz Index for Basic ADLs and the Lawton-Brody Scale for Instrumental ADLs.
These aren't just simple "yes or no" questionnaires. They’re designed to capture the real-world nuances of a person's abilities. The assessment might involve a mix of methods:
- Direct Observation: The professional might watch your loved one perform a simple task, like getting up from a chair or reaching for an item in a cabinet.
- Interviews: They’ll talk with both the individual and their family caregivers to understand daily routines, challenges, and what a typical day looks like.
- Self-Reporting: The person being assessed also gets to share their own perspective on what they find easy or difficult.
This well-rounded approach ensures the final picture is complete, accurate, and truly reflects their day-to-day reality.
The real goal of a formal assessment is to move from subjective feelings to objective facts. It helps turn "I think Dad is having more trouble" into a measurable score that can be used to secure services and track progress.
By using these methods, a care team can pinpoint exactly where support is needed most, which is key to preserving as much independence as possible.
What to Expect During an Evaluation
An ADL assessment is practical and grounded in real-life situations. For the Katz Index of Independence in Activities of Daily Living, the focus is on those six core BADLs. A professional will work to determine if the person is independent or dependent in each area:
- Bathing: Can they get in and out of the tub or shower and wash themselves without help?
- Dressing: Can they pick out their clothes and get fully dressed on their own?
- Toileting: Can they get to and from the toilet, use it, and manage their own hygiene?
- Transferring: Can they move from a bed to a chair and back again without assistance?
- Continence: Can they maintain full control over their bladder and bowel functions?
- Feeding: Can they bring food from their plate to their mouth? (This doesn't include cooking the meal).
The Lawton-Brody IADL Scale digs into the more complex tasks necessary for living alone, like using a telephone, preparing meals, managing finances, or taking medications correctly.
These tools are incredibly reliable. Research shows that scales like these have internal consistency values around 0.95 to 0.98, which basically means the assessments are dependable and trustworthy. You can read the full research on ADL assessment tools to learn more about their clinical validation.
Interpreting the Results for Better Care
The scores from these tools aren't just numbers; they get translated into a functional profile. For instance, the Katz Index gives one point for each ADL the person can handle independently, creating a straightforward score out of six. A lower score clearly signals a greater need for hands-on support.
This objective data is what helps professionals at organizations like NJ Caregiving craft a care plan that actually works. It provides clear answers, guiding everything from how many hours of in-home care are needed to whether home safety modifications are necessary.
Ultimately, a formal assessment ensures that every decision is based on solid evidence, leading to better outcomes and a higher quality of life for your loved one.
Practical Support for ADL Challenges

When an assessment shows that someone you love is starting to struggle with their activities of daily living, it's easy to feel a little overwhelmed. But that moment isn't a time for panic. Instead, it’s a cue to shift your focus toward practical, empowering solutions.
Seeing a decline in ADL abilities doesn't mean an automatic loss of independence. It simply signals that it’s time for some smart adjustments to make daily life safer, easier, and more comfortable. The goal is to bridge the gap between what a person can do and what they need to do. Thankfully, there’s a whole world of support available, from simple home modifications and clever gadgets to professional, hands-on care.
Home Modifications and Assistive Technology
Often, the most powerful support starts right at home with simple, practical changes. These modifications can dramatically lower the risk of falls and make daily tasks far less draining, directly tackling the most common ADL challenges.
A few small but highly effective changes can include:
- Bathroom Safety: Installing grab bars in the shower and beside the toilet is a game-changer for stability. A walk-in shower or a simple bath bench can transform bathing from a risky chore into a safe, less tiring activity.
- Mobility Aids: Just adding handrails in hallways or on staircases can make a world of difference, giving someone the confidence to move around their home securely.
- Kitchen Accessibility: Moving frequently used pots, pans, and dishes to lower, easier-to-reach shelves can make a big impact on meal preparation. Tools like automatic jar openers and utensils with ergonomic grips can also restore a sense of capability in the kitchen.
Beyond physical changes, assistive technology offers targeted help. Automated medication dispensers ensure meds are taken on time, every time, while emergency alert systems (like a medical alert necklace) provide invaluable peace of mind for everyone.
Think of these changes as building a safety net. Each modification and device is another layer of support that empowers a person to navigate their home independently and safely, preserving their autonomy for as long as possible.
These small adjustments can have a massive impact, turning a challenging environment into one that fosters confidence and self-sufficiency.
Professional Support and Therapeutic Services
When home modifications and gadgets aren't quite enough, bringing in professional support is the next logical step. This doesn’t have to mean round-the-clock care. Often, just a few hours of targeted assistance each week can provide the boost someone needs to continue living comfortably at home.
Home Health Aides, like those from a trusted provider such as NJ Caregiving, can assist with personal care tasks like bathing, dressing, and preparing meals. This direct, hands-on help with basic ADLs ensures a person's fundamental needs are met with dignity and respect.
Therapeutic services can also play a huge role in rebuilding or maintaining a person's abilities.
Occupational therapists are the true experts in ADLs. They can teach new, safer ways to perform daily tasks and recommend specific adaptive equipment tailored to an individual's needs. At the same time, physical therapists can design programs to improve strength, balance, and mobility, making essential movements like walking and getting out of a chair much easier.
This professional input is more important than you might think. For instance, getting Medicare to cover a wheelchair often depends on proving the device is necessary to perform ADLs inside the home. This is a perfect example of how central the concept of "what is activities of daily living" is to accessing essential support. Having a therapist to advocate and document these needs can be the key to unlocking those benefits.
By combining practical home solutions with expert professional care, families can build a comprehensive support system. This proactive approach ensures a person gets the right level of assistance to meet their evolving needs, fostering a high quality of life for years to come.
Planning for Future ADL Needs
The absolute worst time to figure out a care plan is right in the middle of a crisis. By thinking ahead while your loved one is still healthy and capable, you can turn a moment of potential panic into a calm, structured process. It's about swapping anxiety for a confident plan for whatever comes next.
This isn't just about logistics; it's about honoring your loved one's wishes. Talking about this early on allows you to create a flexible roadmap that respects their autonomy. The alternative is being forced to make tough decisions for them later on. The goal is to discuss what they want for their care long before it becomes an urgent need.
Starting the Conversation
Bringing up long-term care can feel like a delicate subject. A great way to approach it is by framing the conversation around empowerment—how can we make sure your wishes are followed, no matter what? You’re not discussing a loss of independence, but rather how to best support it for years to come.
A good place to begin is by simply asking what's most important to them. Do they dream of aging in their own home? What are their biggest worries about the future? Opening this dialogue builds a foundation of trust, making the entire planning process a team effort.
Proactive planning is an act of love and respect. It ensures that when the time for more support comes, the decisions are guided by your loved one’s own voice, not by the pressures of an emergency.
Once you’ve opened the door to the conversation, the next step is to tackle the practical side of things: getting the legal and financial pieces in order.
Key Legal and Financial Preparations
Getting crucial documents sorted out is one of the most powerful things you can do. This step ensures someone they trust can manage their affairs if they ever become unable to do it themselves.
- Power of Attorney (POA): This is a legal document that lets your loved one appoint a trusted person to make financial and healthcare decisions on their behalf if they can no longer do so.
- Living Will: This document clearly outlines their preferences for medical treatments, giving family and doctors clear guidance on end-of-life care.
- Long-Term Care Insurance: It's worth exploring policies early. This type of insurance can provide the financial resources to cover in-home care or assisted living, costs that standard health insurance usually won't touch.
Taking these steps provides incredible peace of mind, knowing a solid plan is already in place.
Exploring Future Living Options
Getting familiar with the different care options now helps you make clear-headed choices when the time comes. The "right" choice will depend entirely on an individual’s needs—especially their ability to handle their activities of daily living.
The options are broad, from aging in place with support from a provider like NJ Caregiving to moving into a more specialized community. For instance, if someone mainly needs a hand with IADLs (like cooking or managing medications), in-home care can be the perfect fit. But if basic ADLs become a real struggle, a setting with more hands-on support, such as assisted living or memory care, might be a better and safer choice.
Ultimately, planning ahead gives you a thoughtful strategy that can adapt as needs change. It’s the best way to ensure your loved one gets the right care in a way that truly aligns with what they want for their life.
Of course. Here is the rewritten section, crafted to sound like an experienced human expert while following all your specified requirements.
Common Questions We Hear About ADLs
Even with a good grasp of the basics, you probably still have some questions about how Activities of Daily Living play out in the real world. That's completely normal. Let's walk through some of the most frequent questions we get from families just like yours.
Think of this as the final piece of the puzzle, designed to clear up any lingering confusion and help you feel confident as you start planning for care. These are the kinds of questions that pop up during doctor visits or when you first look into care options, so having the answers ready can make those conversations a lot less stressful.
Who Actually Does an ADL Assessment?
An ADL assessment isn't just an informal chat; it's a structured evaluation that needs to be done by a qualified healthcare professional. This ensures the results are accurate and can be used to build a reliable care plan.
The people you'll most often see performing these assessments are:
- Physicians, especially primary care doctors or geriatricians who specialize in senior health.
- Occupational therapists, who are the true experts in evaluating daily function.
- Physical therapists, focusing on the strength and mobility needed for these tasks.
- Registered nurses, particularly those working in home health or managing hospital discharge plans.
- Social workers or case managers who are coordinating a senior's overall care.
These professionals use standardized tools to keep the evaluation objective. It’s their way of getting a clear, unbiased picture of a person's abilities, which becomes the foundation for all care decisions.
Will Insurance Cover Help with ADLs?
Yes, it often does! In fact, proving that a person needs help with their ADLs is usually the essential first step to unlocking insurance benefits for care. But—and this is a big but—it all comes down to the specifics of your policy or program.
For instance, nearly all long-term care insurance policies require proof that someone can't perform a set number of ADLs (usually two or more) before they'll start paying out.
Understanding your policy's "benefit triggers" is absolutely critical. These triggers are almost always defined by the inability to perform specific Activities of Daily Living, making a formal assessment a non-negotiable step for getting financial help.
Government programs like Medicaid also heavily rely on ADL limitations to determine who is eligible for home and community-based care services. Your best bet is to always review the policy documents yourself or speak directly with a program representative to know exactly what’s required.
What's My First Step if I See a Loved One Struggling?
If you notice a parent or loved one is having a hard time with their daily routine, the single most important first step is to schedule an appointment with their primary care physician. This is the right place to start for a few key reasons.
First, the doctor can run a full check-up to see if a treatable medical issue is behind the decline. Sometimes the culprit is something as simple as a medication side effect or a low-grade infection. If there's no obvious medical cause, the doctor can then refer you to the right specialist—often an occupational therapist—who can perform a detailed functional assessment. From there, you’ll get concrete, expert recommendations for support, home safety improvements, and the right level of care.
At NJ Caregiving, we specialize in providing compassionate, professional support for individuals facing challenges with their Activities of Daily Living. If you're in Princeton, Hamilton, or anywhere in Mercer County and need trusted in-home care, our team is here to help you create a personalized plan that promotes independence and well-being. Learn how our dedicated caregivers can make a difference by visiting https://njcaregiving.com.


