Understanding the Power of Person-Centered Care
Want to see person-centered care in action? This listicle provides seven clear person-centered care examples, demonstrating how this approach improves patient well-being and strengthens provider-patient relationships. Discover how methods like Dementia Care Mapping, Shared Decision-Making, and Patient-Directed Care Plans empower individuals and improve healthcare experiences. These person-centered care examples offer practical insights for seniors, family caregivers, and healthcare professionals alike.
1. Dementia Care Mapping (DCM)
Dementia Care Mapping (DCM) stands as a shining example of person-centered care in action. Developed at the University of Bradford, this structured observational tool places the individual living with dementia at the heart of care planning and delivery. DCM involves meticulously observing and documenting the experiences of people with dementia within their care settings, paying close attention to their well-being and pinpointing factors that either enhance or detract from their quality of life. This approach moves beyond simply providing care tasks and focuses on understanding the individual's emotional and social world. By meticulously analyzing the observed data, care providers gain valuable insights into how to create a more supportive and enriching environment tailored to each person's unique needs and preferences, truly embodying the principles of person-centered care.
DCM employs several key features to achieve its person-centered focus: detailed observation of residents over extended periods, a specific coding system to categorize positive and negative interactions, a structured feedback mechanism for staff development, and an iterative improvement cycle driven by the findings. This systematic approach allows for a deep understanding of the individual's experience and facilitates continuous improvement in care practices.
Why use DCM? DCM provides an evidence-based framework to enhance the lives of individuals with dementia. It shifts the focus from task-oriented care to a deeper understanding of the individual's emotional well-being. This is particularly valuable for family caregivers, professional caregivers in senior services, and hospital discharge planners seeking the best possible care solutions for their loved ones or patients. By understanding the factors that influence well-being, care can be tailored to promote positive experiences and minimize distress.
Examples of Successful Implementation:
- Vida Healthcare (UK): Vida Healthcare uses DCM as a cornerstone of their dementia care approach, demonstrating its effectiveness in a real-world setting.
- St Monica Trust: Implementation of DCM at St Monica Trust led to a remarkable 50% reduction in antipsychotic medication use, highlighting the potential for DCM to improve care and reduce reliance on pharmacological interventions.
- Australian Aged Care Quality Agency: The agency endorses DCM as a valuable tool for elevating the standard of dementia care, further validating its impact.
Pros:
- Evidence-based approach: Extensive research supports the effectiveness of DCM.
- Data-driven improvements: Provides concrete data to guide care adjustments and improvements.
- Empathy development: Helps staff cultivate empathy by experiencing care from the resident's perspective.
- Measurable outcomes: Creates quantifiable outcomes for person-centered care.
Cons:
- Resource-intensive: Requires specialized training and dedicated time for mapping sessions.
- Time-consuming: Proper implementation necessitates a significant time investment.
- Potential for staff discomfort: Staff may initially find being observed intrusive.
- Requires organizational commitment: Actioning the findings requires a commitment from the entire organization.
Tips for Implementation:
- Transparent communication: Begin with a clear communication plan to explain the purpose and benefits of DCM to all staff members.
- Thorough training: Ensure all mappers are well-trained and receive ongoing support.
- Regular mapping sessions: Schedule regular mapping sessions for consistent data collection, rather than relying on one-off observations.
- Constructive feedback: Use findings constructively to drive improvement, not as a punitive measure.
Popularized By:
- Professor Tom Kitwood, founder of person-centered dementia care
- Bradford Dementia Group at University of Bradford
- Dawn Brooker, leading DCM researcher and advocate
DCM deserves its place on this list because it offers a concrete, measurable, and person-centered approach to dementia care. It empowers caregivers with the knowledge and tools to understand the individual's experience and create an environment that truly promotes well-being. While it requires an investment of time and resources, the potential benefits for individuals living with dementia make it a valuable and worthwhile endeavor.
2. Shared Decision-Making (SDM) in Healthcare
Shared Decision-Making (SDM) is a crucial element of person-centered care. It's a collaborative process where healthcare providers and patients work together to make healthcare decisions, considering both clinical evidence and the patient's individual preferences and values. This approach represents a significant shift from traditional, paternalistic models of care, empowering patients to actively participate in their own health journey. Instead of simply receiving instructions, patients engage in a dialogue, exploring options, understanding risks and benefits, and ultimately choosing the path that best aligns with their personal goals and circumstances. This makes SDM a powerful example of person-centered care, placing the individual at the heart of the decision-making process.
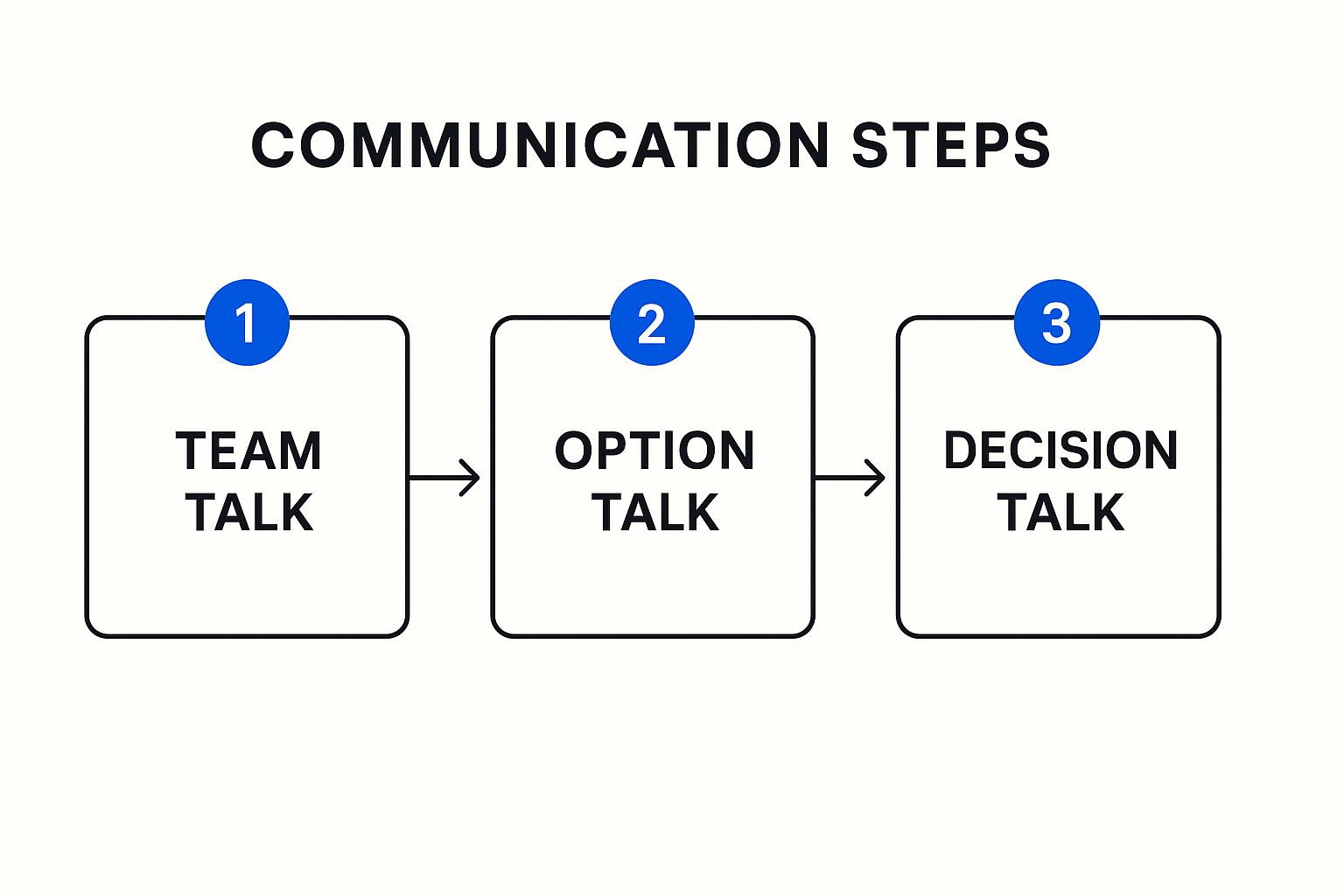
The infographic illustrates the three-talk model of Shared Decision-Making: Team Talk, Option Talk, and Decision Talk. This model provides a structured framework for conversations between healthcare providers and patients. First, in the Team Talk stage, the clinician and patient establish a collaborative relationship, acknowledging the shared responsibility in the decision-making process. Next, during the Option Talk stage, they explore the available options, discussing the potential risks and benefits of each. Finally, in the Decision Talk, the patient considers their values and preferences in light of the available evidence and makes an informed decision. This structured approach ensures that the patient's voice is heard and that decisions are truly shared.
SDM features a structured approach using tools like the three-talk model (Team Talk, Option Talk, and Decision Talk) and patient decision aids. These tools help balance clinical evidence with patient values, leading to more informed decisions. By using visual aids and clearly outlining the options, risks, and benefits, providers can ensure patients, including seniors and their family caregivers at Caring Hands Senior Services, fully understand the information necessary to make an informed choice. This approach is particularly important for complex medical decisions where multiple treatment options exist. For instance, a senior considering different options for managing diabetes can use SDM to weigh the pros and cons of each option, factoring in their lifestyle and preferences.
Pros:
- Increased patient satisfaction and engagement in treatment
- Improved treatment adherence and outcomes
- Reduced decisional conflict and regret
- More appropriate and cost-effective care choices
Cons:
- Can be time-consuming in busy clinical settings
- Requires clinician training and comfort with uncertainty
- May be challenging with patients who prefer directive approaches
- Limited by availability of evidence-based decision aids
Examples of Successful Implementation:
- Mayo Clinic's Shared Decision Making National Resource Center
- Dartmouth-Hitchcock Medical Center's Center for Shared Decision Making
- NHS England's implementation across various clinical pathways
- Veterans Affairs' use of SDM in prostate cancer treatment
Tips for Implementing SDM:
- Use standardized decision aids when available.
- Document patient values and preferences systematically.
- Practice 'teach-back' methods to ensure understanding.
- Schedule adequate time for important decisions.
- Involve family members when appropriate, particularly crucial for seniors utilizing services like Caring Hands Senior Services.
When and Why to Use SDM:
SDM is particularly beneficial when there are multiple treatment options with varying risks and benefits, and when patient preferences play a significant role in the decision. It's essential for building trust and rapport between patients and providers, leading to better health outcomes and increased patient satisfaction. For seniors at Caring Hands Senior Services, SDM can empower them to actively participate in decisions about their care, improving their quality of life and overall well-being.
Key Figures in SDM:
- Dr. Victor Montori at Mayo Clinic
- The Option Grid Collaborative
- International Patient Decision Aid Standards (IPDAS) Collaboration
- Glyn Elwyn, pioneer of the three-talk model
SDM truly deserves its place on this list because it epitomizes person-centered care. By fostering collaboration and respecting patient autonomy, SDM empowers individuals to make informed decisions that align with their values and preferences, ultimately leading to better health outcomes and a more positive healthcare experience. This is especially relevant for the diverse population served by Caring Hands Senior Services, ensuring each individual receives care tailored to their unique needs and wishes.
3. Patient-Directed Care Plans: Empowering Individuals in Their Healthcare Journey
Patient-directed care plans are a powerful example of person-centered care, placing the individual firmly at the helm of their own healthcare journey. This approach shifts the traditional dynamic, moving away from clinician-driven decisions towards a collaborative model where patients actively participate in shaping their care. Instead of simply receiving prescribed treatments, individuals become active partners, working with their care team to create a customized healthcare roadmap that aligns with their personal values, preferences, and goals. This is particularly relevant for Caring Hands Senior Services' target demographics, including seniors aging in place, those with chronic illnesses, and their family caregivers.
How Patient-Directed Care Plans Work:
These comprehensive documents outline a variety of crucial elements:
- Health Goals: Specifically defined, measurable, achievable, relevant, and time-bound objectives that the patient wants to achieve. For a senior with diabetes, this might be maintaining a specific blood sugar range or increasing mobility.
- Treatment Preferences: Clearly articulated choices about the types of treatments the patient is willing or unwilling to undergo. This could involve preferences for medication, therapy, or other interventions.
- Coping Strategies: Methods the patient uses to manage their condition, including stress reduction techniques, pain management strategies, and emotional support systems. For family caregivers, this might involve respite care options offered by Caring Hands Senior Services.
- Personal Values: Fundamental beliefs and principles that guide the patient's decision-making process. This might include religious beliefs, cultural practices, or personal philosophies about health and well-being.
- Emergency and Contingency Planning: Instructions for handling unexpected health events or changes in condition. This is especially important for seniors with chronic illnesses and can provide peace of mind for their families.
Features of Effective Patient-Directed Care Plans:
- Collaborative Development: Created through a partnership between the patient, their family (where appropriate), and the care team, including physicians, nurses, therapists, and social workers.
- Focus on Quality of Life: Prioritizes not only clinical outcomes but also the patient's overall well-being and ability to live a fulfilling life.
- Regular Review and Updates: Dynamic documents that are reviewed and adjusted as needed based on the patient's changing health status, preferences, or goals.
- Holistic Approach: Integrates non-medical factors like social support, spiritual needs, and emotional well-being.
- Accessibility: Ideally, easily accessible to the patient and their authorized caregivers, potentially through digital platforms.
Benefits of Patient-Directed Care Plans:
- Increased patient ownership and engagement in their treatment
- Improved adherence to treatment plans
- Enhanced communication between providers and patients
- Reduced unnecessary interventions and healthcare costs
- Greater continuity of care across different settings
- Improved patient satisfaction and quality of life
Challenges of Patient-Directed Care Plans:
- Time-intensive development process
- Potential conflicts between patient preferences and clinical best practices
- Need for consistent updating as conditions change
- Integration with electronic health records can be challenging
Examples of Successful Implementation:
- Kaiser Permanente's Coordinated Care Plan approach
- Geisinger Health's integration of Patient-Generated Health Data
- PACE (Program of All-inclusive Care for the Elderly) individualized care plans
- UK's Personal Health Budgets program
Tips for Implementing Patient-Directed Care Plans:
- Use standardized templates that can be personalized to each individual.
- Incorporate "teach-back" methods to ensure patients understand their plan.
- Schedule regular reviews, especially following significant health events.
- Include advance care planning discussions as part of the process.
- Make plans easily accessible to patients, ideally through digital platforms.
Why Patient-Directed Care Plans Deserve a Place on This List:
Patient-directed care plans epitomize person-centered care by empowering individuals to actively participate in their healthcare. This approach leads to improved outcomes, greater patient satisfaction, and a stronger therapeutic alliance between patients and their care team. For Caring Hands Senior Services, this model can be particularly valuable for demonstrating a commitment to individualized care and fostering trust with clients and their families. By focusing on the specific needs and preferences of each senior, Caring Hands Senior Services can ensure that its care plans are not only clinically sound but also deeply respectful of individual autonomy and quality of life.
4. The Green House Project Model
The Green House Project Model stands as a compelling example of person-centered care, offering a radical departure from the traditional institutional feel of nursing homes. This model prioritizes creating small, intimate living environments designed to feel like real homes, fostering a sense of community and belonging for its residents. Instead of long hallways and sterile environments, Green House homes typically accommodate 10-12 elders, emphasizing meaningful relationships, empowered staff, and individualized care plans tailored to each resident's unique preferences and routines. This approach aims to empower residents to live full and meaningful lives within a supportive and nurturing community.

Several key features distinguish the Green House model: small-scale facilities designed like actual homes; private rooms and bathrooms for all residents, offering privacy and dignity; specially trained universal workers, called Shahbazim, who provide holistic care, from direct care and meal preparation to household management; and a flattened hierarchy that empowers direct care staff with significant autonomy in decision-making. These homes also incorporate dedicated spaces for communal dining and activities, fostering social interaction and a sense of community. This model is particularly relevant for seniors and elderly individuals who desire a home-like setting, those suffering from chronic illnesses requiring specialized care, and family caregivers seeking an alternative to traditional nursing homes.
The Green House Project boasts several notable advantages. Residents often report higher satisfaction and an improved quality of life. Studies have also shown lower rates of hospitalization and pressure ulcers, suggesting better overall health outcomes. Furthermore, the model fosters a positive work environment for staff, resulting in reduced turnover and increased job satisfaction. This directly translates to more personalized care and the development of deeper relationships between staff and residents. Notably, the design of Green House homes has demonstrated improved infection control, a critical factor highlighted during the COVID-19 pandemic.
However, implementing the Green House model also presents challenges. Initial construction costs per bed can be higher than traditional facilities. The model necessitates a significant organizational culture change, often requiring a shift in mindset and operational procedures. Training universal workers effectively is crucial for successful implementation and can be demanding. Furthermore, regulatory hurdles in some states can pose challenges to adoption. Finally, while staff satisfaction increases, staffing costs may also be higher due to the higher staff-to-resident ratio.
Successful examples of the Green House Project Model include the Leonard Florence Center for Living in Chelsea, MA, St. John's Home in Rochester, NY, The Eddy Village Green in Cohoes, NY, and John Knox Village in Pompano Beach, FL. These facilities demonstrate the positive impact of the model on resident well-being and staff satisfaction. For families and healthcare professionals seeking person-centered care options, these examples offer valuable insights.
For those considering implementing the Green House Project Model, several tips can guide the process: Secure organizational leadership commitment to culture change from the outset. Involve direct care staff in planning and design decisions to foster ownership and buy-in. Provide comprehensive training on person-centered philosophies to ensure staff embody the model's core values. Plan the transition carefully when converting from traditional models to minimize disruption. Finally, establish feedback systems to continuously refine practices and adapt to the evolving needs of residents and staff. The Green House Project, popularized by Dr. Bill Thomas, with initial funding from The Robert Wood Johnson Foundation, NCB Capital Impact (now Capital Impact Partners), and The Center for Innovation (TMCFI), exemplifies a commitment to truly person-centered care, earning its place on this list for its transformative approach to elder care.
5. Motivational Interviewing in Healthcare
Motivational Interviewing (MI) stands as a shining example of person-centered care in action. It’s a collaborative, goal-oriented counseling style designed to strengthen a patient's own motivation and commitment to changing health behaviors. Unlike traditional approaches where clinicians might offer direct advice, MI empowers patients to explore their ambivalence towards change and discover their own reasons and methods for improvement. This approach perfectly embodies person-centered care by prioritizing the patient's autonomy, values, and lived experience.
Instead of telling patients what to do, MI practitioners guide them through a process of self-discovery. They act as facilitators, helping patients identify their internal resources and build confidence in their ability to achieve their goals. This makes MI particularly effective for complex behavioral changes, like managing chronic conditions, adhering to medication regimens, or adopting healthier lifestyle choices. For families and caregivers seeking to support their loved ones, understanding the principles of MI can be invaluable.
How Motivational Interviewing Works:
MI operates on four core processes:
- Engaging: Building a trusting and respectful relationship with the patient.
- Focusing: Collaboratively defining the target behavior for change.
- Evoking: Eliciting the patient's own motivations for change and exploring their perceived benefits and drawbacks.
- Planning: Developing a concrete action plan based on the patient’s identified motivations and resources.
These processes are supported by the "OARS" skills:
- Open Questions: Encouraging thoughtful responses rather than simple yes/no answers.
- Affirmations: Recognizing and validating the patient’s strengths and efforts.
- Reflective Listening: Demonstrating understanding and empathy by reflecting back the patient’s statements.
- Summarizing: Pulling together key points to ensure shared understanding and guide the conversation.
Why Motivational Interviewing Deserves its Place on this List:
MI is more than just a conversation; it's an evidence-based approach proven effective across various health behaviors, from smoking cessation and substance use disorders to diabetes management and medication adherence. Its focus on patient autonomy and empowerment fosters intrinsic motivation, leading to more sustainable change than directive approaches.
Examples of Successful Implementation:
- Veterans Health Administration: Nationally implemented MI for substance use disorders.
- NHS Health Scotland: Adopted MI for smoking cessation programs.
- Cleveland Clinic: Integrated MI into diabetes self-management programs.
- Kaiser Permanente: Utilizing MI in medication adherence counseling.
Pros:
- Evidence-based effectiveness.
- Can be delivered in brief interventions (15-30 minutes).
- Reduces resistance and defensiveness.
- Builds intrinsic motivation for sustainable change.
- Applicable across diverse cultural contexts.
Cons:
- Requires significant practitioner training and practice.
- May feel slow to practitioners used to giving direct advice.
- Less structured than some interventions, requiring clinical judgment.
- Not appropriate for all clinical situations (e.g., acute emergencies).
Actionable Tips for Family Caregivers and Healthcare Professionals:
- Focus on reflective listening: Practice accurately reflecting the patient's feelings and perspectives.
- Respond to "sustain talk" (resistance to change) without confrontation: Acknowledge the patient's concerns and explore their ambivalence.
- Use decisional balance exercises: Help the patient weigh the pros and cons of change.
- Record sessions (with permission) for self-review: Identify areas for improvement in your MI skills.
- Participate in ongoing supervision or coaching: Refine your technique and receive expert feedback.
Motivational Interviewing empowers individuals to take ownership of their health journey. By focusing on the individual's internal resources and wisdom, MI fosters lasting behavior change and exemplifies the core principles of person-centered care. For Caring Hands Senior Services, incorporating MI into care plans can significantly benefit both the seniors they serve and their families, promoting better health outcomes and a stronger sense of self-efficacy in managing health challenges.
6. Person-Centered Care Planning in Mental Health
Person-centered care planning in mental health represents a fundamental shift from traditional, deficit-focused treatment models. Instead of primarily focusing on diagnoses and symptoms, this approach prioritizes the individual's unique strengths, preferences, and recovery goals. It empowers individuals to take an active role in directing their own recovery journey, with mental health professionals acting as collaborative partners and facilitators rather than solely as authority figures. This model acknowledges that true healing and well-being come from within and are best achieved when the individual feels heard, respected, and in control of their own care.

Person-centered planning works by actively involving the individual in every step of the planning process. This includes identifying personal recovery goals, exploring available resources and supports, and developing a plan that aligns with their values and aspirations. Recovery-oriented language, which emphasizes possibilities and strengths, is essential. Documentation is created collaboratively, with client input and approval, ensuring transparency and ownership. The focus shifts from managing symptoms to building resilience, fostering hope, and connecting individuals with natural supports and community resources. Regular reviews and adjustments are made based on the individual's evolving needs and preferences, ensuring the plan remains dynamic and relevant. Trauma-informed practices, prioritizing safety and choice, are integrated throughout the process.
Examples of successful person-centered care planning implementations:
- CommonGround program developed by Pat Deegan: This program empowers individuals to create and share their own recovery stories, fostering self-advocacy and connection.
- Recovery Care Planning at Thresholds in Chicago: This organization emphasizes community integration and peer support in their person-centered planning process.
- Connecticut's statewide Recovery-Oriented Systems of Care: This initiative demonstrates how person-centered principles can be applied system-wide, impacting policy and service delivery.
- New York State Office of Mental Health's Recovery Planning Initiative: This program promotes shared decision-making and individualized care planning across the state.
Actionable Tips for Implementing Person-Centered Care:
- Use person-first language: Refer to individuals as "people with schizophrenia" rather than "schizophrenics." This small change promotes respect and acknowledges their individuality.
- Implement shared decision-making support tools: Provide resources that help individuals weigh options and make informed choices about their care.
- Create libraries of strength-based goal statements: Offer examples of positive, achievable goals to inspire and guide individuals in their planning process.
- Involve peers in the care planning process when possible: Peer support specialists can offer valuable insights and encouragement.
- Schedule planning meetings at times convenient for the person: This demonstrates respect for their time and priorities.
- Consider using visual tools for those who prefer non-verbal planning: Visual aids can enhance communication and understanding.
Why Use Person-Centered Care Planning?
This approach is particularly valuable for individuals with mental health conditions because it fosters hope, promotes self-determination, and recognizes the individual's inherent capacity for recovery. It can be applied across various settings, including inpatient units, community mental health centers, and private practice.
Pros:
- Improved treatment engagement and adherence
- Greater sense of empowerment and self-efficacy
- Better alignment between provider and client goals
- Higher rates of achieving personally meaningful outcomes
- Reduced use of coercive interventions
Cons:
- May conflict with insurance documentation requirements
- Time-intensive, especially in initial stages
- Requires organizational culture shift and staff training
- Can be challenging to implement in crisis situations
Person-centered care planning in mental health deserves its place on this list because it represents a best-practice approach that has been shown to significantly improve outcomes for individuals experiencing mental health challenges. It aligns perfectly with Caring Hands Senior Services' focus on individual needs and empowering individuals to live fulfilling lives, especially for those dealing with chronic illnesses like dementia and Alzheimer's, where person-centered care is crucial. By shifting the focus from illness to individual strengths and preferences, this approach fosters a more hopeful and empowering recovery journey. While implementation requires a dedicated commitment to training and cultural change, the long-term benefits of increased engagement, improved outcomes, and greater client satisfaction make it a worthwhile investment for any organization committed to providing high-quality, person-centered care.
7. Patient and Family Advisory Councils (PFACs): A Cornerstone of Person-Centered Care
Patient and Family Advisory Councils (PFACs) represent a powerful example of person-centered care in action. They are formal structures that bring the patient and family voice directly into the heart of healthcare organizations, influencing governance, design, and daily operations. By actively involving those who have experienced care firsthand, PFACs ensure services are truly patient-centered, meeting the needs and preferences of the individuals they serve. This approach aligns perfectly with the mission of organizations like Caring Hands Senior Services, which prioritizes client well-being and family involvement.
How PFACs Work:
PFACs consist of patients and family members who have received care at the organization. These advisors work collaboratively with staff on various aspects of care delivery, from improving the physical environment and refining policies to shaping programs and enhancing the overall patient experience.
Key Features of Effective PFACs:
- Regular Meetings with Structure: Formal meetings with established agendas, leadership roles, and clear objectives ensure productive discussions and actionable outcomes.
- Diverse Membership: A council reflective of the patient population ensures that diverse perspectives and needs are considered. For Caring Hands Senior Services, this might include representation from different age groups, cultural backgrounds, and levels of care needs within their client base.
- Defined Roles and Responsibilities: Clear expectations for members and staff, including terms of service, facilitate effective collaboration and prevent misunderstandings.
- Direct Reporting Lines: A direct reporting pathway to organizational leadership ensures that PFAC recommendations are heard and considered at the highest levels.
- Involvement in Strategic Planning and Daily Operations: PFACs contribute to both long-term strategy and day-to-day improvements, ensuring a consistent focus on patient needs.
- Collaborative Work on Improvement Projects: PFACs often participate in specific projects aimed at enhancing care delivery, such as redesigning patient intake processes or improving communication between caregivers and families.
Benefits of Implementing PFACs:
- Authentic Patient Voice: PFACs provide invaluable insights into the patient experience, identifying areas for improvement that staff might overlook. This is particularly crucial for Caring Hands Senior Services, allowing them to tailor services to the specific needs of their clients.
- Proactive Problem Solving: By identifying potential issues early on, PFACs can help organizations avoid costly mistakes in facility design, program implementation, and service delivery.
- Stronger Community Relationships: PFACs foster trust and open communication between the organization and the community it serves, building strong relationships and enhancing reputation. This resonates strongly with Caring Hands Senior Services' focus on community engagement.
- Enhanced Patient Satisfaction: By actively involving patients and families in shaping care delivery, PFACs contribute to greater patient satisfaction and improved outcomes.
Challenges and Considerations:
- Resource Commitment: Establishing and maintaining a PFAC requires dedicated staff support, time, and resources.
- Meaningful Integration: PFACs can become symbolic rather than impactful if their recommendations are not integrated into organizational operations.
- Potential for Conflict: Differences of opinion between advisors and administrators may arise. Establishing clear processes for addressing these disagreements is crucial.
- Membership Recruitment: Recruiting and retaining a diverse and representative membership can be challenging.
Tips for Successful PFAC Implementation:
- Provide Comprehensive Training: Equip new members with the knowledge and skills they need to contribute effectively.
- Foster Collaboration: Ensure staff understands the importance of collaborative partnerships with PFAC members.
- Set Clear Expectations: Define roles, responsibilities, and time commitments upfront.
- Track and Communicate Impact: Demonstrate the value of PFAC contributions by tracking and sharing the results of their recommendations.
- Consider Compensation: When feasible, compensating advisors for their time and expertise acknowledges their valuable contributions.
Examples of Successful PFACs:
Organizations like Dana-Farber Cancer Institute, Georgia Health System, Children's Hospital of Philadelphia, and Kaiser Permanente have successfully implemented PFACs, demonstrating their value in improving patient care. These examples can offer valuable insights for Caring Hands Senior Services as they consider implementing their own PFAC.
Why PFACs Deserve a Place on this List:
PFACs embody the core principles of person-centered care by placing patients and families at the center of decision-making. They provide a vital mechanism for continuous improvement, ensuring that healthcare organizations are truly responsive to the needs of those they serve. For Caring Hands Senior Services, a PFAC can be a powerful tool for strengthening their commitment to person-centered care and enhancing the lives of their clients and their families.
7 Key Person-Centered Care Examples Compared
| Approach | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Dementia Care Mapping (DCM) | High: specialized training, time-consuming, iterative cycles | High: trained mappers, organizational commitment | Improved person-centered care, measurable quality of life gains | Dementia care settings needing detailed behavioral insights | Empathy development, evidence-backed improvements |
| Shared Decision-Making (SDM) | Moderate: clinician training, structured 3-talk model | Moderate: decision aids, clinician time | Increased patient engagement, better adherence, reduced regret | Clinical decisions requiring patient value integration | Enhances autonomy, improves satisfaction and cost-effectiveness |
| Patient-Directed Care Plans | Moderate-High: collaborative, requires regular updates | Moderate: time for collaboration and review | Greater patient ownership, aligned care with patient values | Personalized chronic and long-term care planning | Improves communication, continuity across settings |
| The Green House Project Model | High: requires culture change, new staffing models, construction | High: facility redesign and staff training | Higher resident satisfaction, reduced hospitalizations, better staff retention | Long-term elder care seeking homelike environment | Personalized care, empowered staff, improved infection control |
| Motivational Interviewing | Moderate-High: requires training and practice to master skills | Moderate: trained practitioners, supervision | Builds motivation, reduces resistance, supports sustainable change | Behavior change counseling across health behaviors | Effective brief interventions, culturally adaptable |
| Person-Centered Care Planning | High: time-intensive, ongoing review, culture shift | Moderate-High: staff training and documentation | Improved engagement, empowerment, meaningful recovery outcomes | Mental health recovery-focused treatment | Strength-based, trauma informed, client-directed |
| Patient and Family Advisory Councils (PFACs) | Moderate-High: formal structure, ongoing integration | Moderate-High: staff support, diverse membership | Authentic patient input, improved policies, increased trust | Organizational governance and quality improvement | Patient voice integration, uncovers blind spots, community trust |
Taking Action: Implementing Person-Centered Care
This article explored several powerful person-centered care examples, from Dementia Care Mapping and Shared Decision-Making to the innovative Green House Project model and the engagement fostered by Patient and Family Advisory Councils. These diverse approaches all share a common thread: prioritizing individual needs, preferences, and values in all aspects of care. By understanding and implementing these strategies, healthcare providers and family caregivers alike can create a more responsive, respectful, and ultimately, more effective care experience.
The most crucial takeaway is that person-centered care is not a one-size-fits-all approach. It requires active listening, empathy, and a willingness to adapt care plans to the unique circumstances of each individual. Mastering these concepts goes beyond simply improving patient satisfaction; it empowers individuals to take an active role in their own well-being, leading to better health outcomes and a greater sense of dignity and control. Implementing person-centered care requires a commitment to holistic well-being, encompassing not just physical health but also mental and emotional wellness. For a deeper understanding of this integrated approach, consider exploring resources like Well-being Mastery: Proven Strategies from Whelm on achieving true well-being.
Ultimately, person-centered care is about recognizing the inherent worth of every individual and creating an environment that supports their unique journey toward health and well-being. Embracing these principles leads to a more compassionate and effective approach to care that benefits both the individual and the entire caregiving ecosystem. If you're seeking personalized senior care services in Mercer County, including Hamilton and Princeton, NJ, that prioritize person-centered care, Caring Hands Senior Services provides compassionate support tailored to individual needs and preferences, empowering seniors to live fulfilling lives while respecting their autonomy and dignity. Contact us today to learn how we can help.



