If you’re a primary caregiver, you know it's a role that demands everything you have—physically, mentally, and emotionally. It's often described as a marathon, not a sprint. But even marathon runners need water breaks. That's essentially what Medicaid respite care is: a planned, temporary break for you.
It’s a structured service designed to give you relief, prevent burnout, and let you manage your own life, all while knowing your loved one is still getting professional, compassionate care.
A Lifeline for Family Caregivers

To sustain the long-term commitment of caregiving, you simply have to have opportunities to rest and recharge. Medicaid respite care is the support system that makes this possible, acting as a true lifeline for families.
This isn’t about finding a last-minute babysitter. It’s a formal benefit that allows you to step away with complete confidence. Whether you need to run to your own doctor's appointment, handle errands, or just take a few quiet hours for yourself, a qualified professional steps in. This service is fundamental to making long-term in-home care a sustainable choice for families, which is often far better and more affordable than moving a loved one into a facility.
How Does It Actually Work?
The whole point of Medicaid respite care is to provide temporary relief, and this can happen in a few different ways. The specific options you have will really depend on your state's Medicaid program and your loved one's unique needs.
Some of the most common forms of respite care include:
- In-Home Assistance: A certified aide comes directly to your home for a set number of hours to take over all care duties.
- Out-of-Home Care: Your loved one might attend an adult day care center or another community-based program for a day.
- Short-Term Stays: In some situations, respite can cover a brief stay in a certified facility, like a nursing home or assisted living center.
This flexibility is key. It lets families pick the option that best fits their schedule and situation, ensuring the person receiving care is comfortable and the primary caregiver gets a meaningful, restorative break.
Widespread Recognition of Its Importance
The value of respite care isn’t just an anecdotal idea; it’s a recognized necessity in our healthcare system. In 2022, a huge majority of states—47 states plus the District of Columbia—included respite care coverage in their Medicaid Home and Community-Based Services (HCBS) waivers for older adults and people with physical disabilities.
This widespread adoption sends a clear message: supporting family caregivers is essential for community-based health. You can learn more about these emerging respite strategies in Medicaid waivers and see how states are helping families all across the country.
This structured support is more than just a "break." It’s a preventative measure that protects the health and well-being of the entire family, allowing caregivers to keep providing loving care without sacrificing their own health in the process.
For a quick overview, the table below breaks down the essentials of this vital service.
Medicaid Respite Care At a Glance
| Aspect | Description |
|---|---|
| Primary Goal | To provide temporary relief to unpaid primary caregivers to prevent burnout. |
| Who It's For | Families where one person is the main caregiver for a Medicaid-eligible individual. |
| Service Setting | Can be provided in the home, at an adult day care, or in a facility. |
| Funding Source | Covered through specific state Medicaid programs, usually HCBS waivers. |
| Key Benefit | Enables sustainable long-term care at home and supports caregiver health. |
Ultimately, respite care acknowledges the immense contribution of family caregivers and gives them the support they need to continue their incredible work.
It’s easy to call caregiving a marathon, but that analogy doesn't quite hit the mark. A marathon has a clear finish line. Caregiving is a journey that stretches on, demanding incredible emotional and physical stamina day after day. The real value of Medicaid respite care isn’t just about getting a simple break; it’s about providing the essential support that keeps the whole journey from falling apart.
For the caregiver, this planned relief is nothing short of a lifeline. It’s that critical, scheduled time to catch your breath, take care of your own health, and stop the slow burn of chronic stress that wears down so many. For the person receiving care, it often means new social interactions and ensures their support is coming from someone who is rested, patient, and fully present.
A Day Transformed by Respite
To really get it, let's look at a typical day for a family caregiver—first without respite, and then with it.
Without that support, the day can feel like a relentless cycle. It starts with exhaustion and runs through a non-stop schedule of managing medications, preparing meals, helping with personal care, and providing emotional support. The caregiver's own needs, whether it's a routine doctor's appointment or just a coffee with a friend, get pushed aside again and again. This isn't just tough; it's unsustainable and the fast track to caregiver burnout—a state of total physical, mental, and emotional exhaustion.
Now, imagine that same day with just a few hours of professional respite care. A trained caregiver arrives, and the family caregiver can step away, completely guilt-free. They can finally go to that overdue check-up, run errands without constantly checking the clock, or just sit in a park and be still for a moment. This isn't a luxury. It's a fundamental part of providing good care. That short break allows them to come back refreshed and better able to offer the patient, compassionate support their loved one deserves.
The Broader Impact on Health and Costs
The benefits of Medicaid respite care create a powerful ripple effect that goes far beyond the family home, touching the entire healthcare system. When caregivers are supported, the quality and consistency of at-home care get a major boost. This proactive approach helps stop crises before they start, leading to much better health outcomes and, surprisingly, big cost savings.
Investing in a caregiver's well-being is a direct investment in the health of the person they are caring for. It's a preventative measure that keeps families together and reduces the strain on emergency medical services.
This isn't just a nice idea; the numbers prove it. A landmark 2012 study looked at Medicaid records for over 28,000 children with autism and found a stunning connection. For every $1,000 states invested in respite care over 60 days, the chance of a child needing hospitalization dropped by 8%. It shows that respite is more than just a helping hand—it's a critical intervention that prevents expensive medical emergencies. You can read more about these respite care findings and what they mean for public health.
Connecting Personal Wins to Systemic Advantages
Every personal win that respite care makes possible—a caregiver feeling recharged, a loved one smiling after a pleasant visit—is a building block for a stronger, more efficient healthcare system.
- Reduced Hospital Readmissions: A supported caregiver is simply better prepared to manage complex health needs at home, preventing the kinds of complications that often lead to a return trip to the hospital.
- Delayed Need for Institutional Care: By making care at home manageable for the long haul, respite services can delay or even avoid the need for far more expensive nursing home or long-term care facility placements.
- Improved Mental Health: Caregivers who use respite services consistently report lower levels of depression, anxiety, and stress, which lifts the mood and improves the dynamic for the entire family.
At the end of the day, Medicaid respite care is based on a simple truth: you can't pour from an empty cup. By providing these essential breaks, the system empowers families to keep providing high-quality, loving care at home, creating a healthier, more stable situation for everyone involved.
Understanding Eligibility for Respite Care

When you start looking into Medicaid respite care, it's easy to assume there's a single box to check. The reality is a bit more involved. Think of it like a two-part key needed to unlock this vital support for your family. Both parts have to fit perfectly, and knowing what they are from the get-go can save you a lot of guesswork and frustration.
Here's the breakdown: First, the person needing care has to be eligible for your state's Medicaid program, both financially and medically. Second, there must be a primary, unpaid caregiver who genuinely needs a break from their duties. These two pieces work hand-in-hand to make sure the program helps the families who need it most.
The Role of Medicaid Waivers
Most states don't offer respite care through their standard Medicaid plan. Instead, they use special programs called Home and Community-Based Services (HCBS) waivers. The simplest way to picture an HCBS waiver is to think of it as a special ticket.
Your regular Medicaid plan is like a general admission ticket to an amusement park—it gets you in the gate and covers the basic medical services. But some of the best attractions, like respite care, require an extra pass. The HCBS waiver is that pass, giving you access to services that allow your loved one to receive care at home instead of in a nursing facility.
This waiver system is the foundation of Medicaid respite care. It's the state's way of acknowledging that supporting the caregiver is just as critical as supporting the person they care for. It helps keep families together and improves everyone's quality of life.
For most families, getting into one of these waiver programs is the main pathway to having Medicaid fund your respite services.
Who Is Considered the Care Recipient?
Before respite care is even on the table, the person needing support has to qualify for an HCBS waiver in their state. This usually comes down to two different assessments.
- Financial Assessment: This is a close look at the individual's income and assets. The goal is to confirm they meet the state’s financial limits for Medicaid. These numbers can change quite a bit from one state to another, so it's important to check your local requirements.
- Medical or Functional Assessment: A healthcare professional, typically a nurse or social worker, will evaluate your loved one's care needs. They’ll look at how much help is needed with Activities of Daily Living (ADLs)—things like bathing, dressing, and eating—to see if they require a level of care similar to what a nursing home would provide.
Once someone is approved for Medicaid and enrolled in the right HCBS waiver, the door to respite care opens. The entire point is to establish that the individual has a real, ongoing need for long-term support.
How States Assess the Need for Caregiver Relief
After the care recipient's eligibility is confirmed, the focus turns to the caregiver. The state needs to verify that there is indeed an unpaid, primary caregiver who is handling the bulk of the responsibilities and needs relief.
This isn't about judging your abilities as a caregiver. It’s the opposite—it’s a formal acknowledgment of the incredible amount of work you do every day. A case manager will likely sit down with you to talk about your caregiving schedule, what your duties involve, and the toll it’s taking on your own well-being. This conversation is key because it helps them decide how many respite hours your family will be approved for.
This final step ensures the Medicaid respite care program does what it’s designed to do: prevent caregiver burnout and keep the entire in-home care situation stable and healthy. For families in New Jersey trying to figure all this out, getting expert help can be a real game-changer. At NJ Caregiving, we guide families in Mercer County through these requirements so they know exactly what to expect.
How to Apply for Medicaid Respite Services
Let's be honest: applying for Medicaid respite care can feel like trying to solve a puzzle with half the pieces missing. The process often involves multiple steps, a mountain of specific paperwork, and waiting periods that can test anyone’s patience.
The key is to break it all down into manageable stages. When you do, what seems like a bureaucratic maze turns into a clear, step-by-step path forward. Getting these vital services usually comes down to three main phases: getting approved for Medicaid itself, enrolling in the right waiver program, and finally, completing a needs assessment.
The First Step: Applying for Medicaid
Before you can even think about respite services, the person needing care has to be enrolled in your state's Medicaid program. This is the absolute foundation. The application will dig into two key areas: their financial situation and their medical need for care.
Having your documents in order ahead of time can make a world of difference and speed things up considerably. You’ll want to gather:
- Proof of Income: This includes recent pay stubs, Social Security benefit statements, or any pension records.
- Asset Documentation: Pull together bank statements, property deeds, and information on any stocks or bonds.
- Personal Identification: Make sure you have birth certificates, Social Security cards, and proof of state residency handy.
Once you submit the application, your state’s Medicaid agency will review everything to make sure your loved one meets the strict income and asset limits. Getting this initial approval is the gateway to everything else.
This image shows a simplified view of the journey to secure respite care.
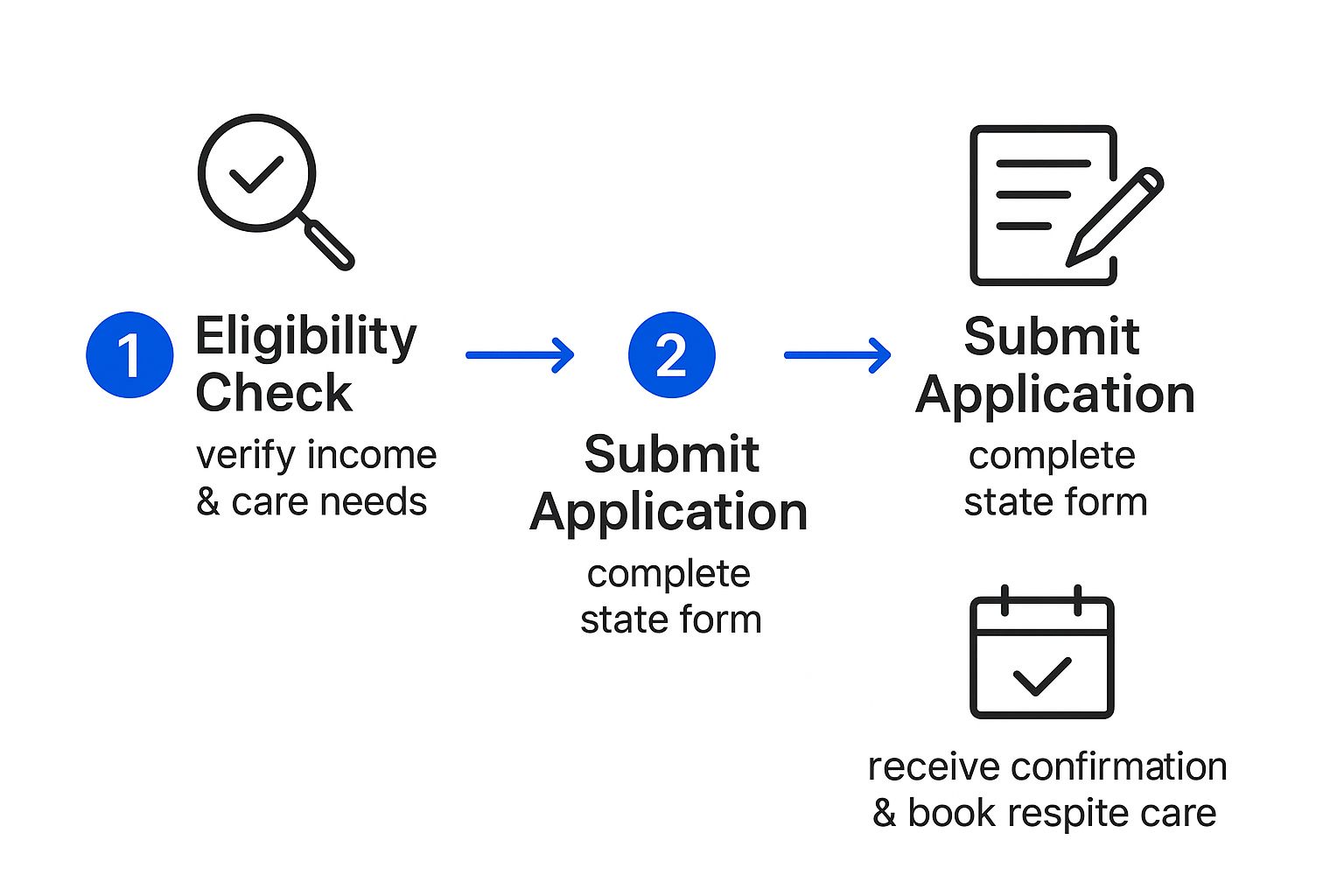
As you can see, proving eligibility is the critical starting point before an application can even lead to scheduling that much-needed break.
Finding the Right HCBS Waiver
Once Medicaid is approved, the next move is to enroll in a Home and Community-Based Services (HCBS) waiver. These waivers, as we've talked about, are the special programs that actually fund services like respite care. This is often where things get tricky, because many waivers have long waiting lists. We’re talking thousands of people in some states, with waits that can stretch on for years.
Don't let a waiting list discourage you. It is absolutely crucial to get your loved one's name on that list as soon as you possibly can, even if the wait seems impossibly long. While you wait, you can look into other state programs or local non-profits that might offer caregiver support in the meantime.
To find the right waiver, your best bet is to contact your state’s Medicaid office or your local Area Agency on Aging. They can walk you through which waivers are available and help you figure out which one best fits your loved one’s situation, whether it’s for an older adult, someone with a developmental disability, or a person with specific medical conditions.
The Needs Assessment and Advocating for Hours
When a spot on a waiver finally opens up, a case manager will reach out to schedule a needs assessment. Think of this as a detailed interview and evaluation to figure out the exact level of care required—and, most importantly, the number of respite hours your family will be granted. The case manager will want to talk with both you and your loved one.
This is your moment to advocate for your family. Be completely honest and thorough when you describe your caregiving duties and the toll they take.
Key Questions to Prepare For:
- How many hours a day are you spending on direct care tasks?
- Does your loved one require supervision around the clock?
- How has caregiving impacted your own health, your job, and your personal life?
- What are your biggest challenges? (e.g., heavy lifting, managing difficult behaviors)
Your answers are what help the case manager build a complete picture of your situation. This isn't the time to downplay your struggles; this assessment is what determines the amount of support you'll get. For families in Mercer County, this can feel like a lot to handle, but organizations like NJ Caregiving can provide guidance to ensure you are fully prepared to secure the Medicaid respite care you truly deserve.
How Respite Care Programs Vary By State
One of the biggest misconceptions about Medicaid respite care is that it's a one-size-fits-all national program. It’s actually a partnership between the federal government and each individual state. This means the rules, the benefits, and the way you get services can look completely different depending on which side of a state line you're on.
Think of it like this: the federal government provides the basic recipe, but each state is its own chef, free to add local ingredients or adjust the portion sizes based on its own budget and priorities. This structure gives states flexibility, but it creates a complex and often confusing system for families to navigate. What's a standard benefit in one state might be severely limited or not even offered in another. That's why doing your local homework isn't just a good idea—it's absolutely essential.
Why Services and Budgets Differ
So, why the huge differences? It really boils down to money and priorities. States have a lot of say in how they spend their Medicaid funds, particularly through their Home and Community-Based Services (HCBS) waivers. The hard truth is that state budgets for respite services are often surprisingly small.
In fact, data shows that the median share of total 1915(c) waiver funding that states put toward respite care is just 0.49%. It’s a tiny slice of the pie, meaning most states dedicate very little of their Medicaid waiver budgets to giving family caregivers this vital break. You can discover more about state respite care spending to see how these allocations play out across the country.
This limited funding often translates directly into stricter limits on service hours, narrower provider choices, and longer waiting lists. It’s a crucial piece of information that helps set realistic expectations for families starting this journey.
Knowing this from the start helps you understand why it's so important to be a strong advocate for your family's needs during the entire assessment and application process.
State-by-State Program Differences
The differences between states go way beyond just the number of hours you can get. They can touch every single part of your respite care experience.
To really illustrate this point, let’s look at how two hypothetical states might set up their programs. This is just an example, but it shows exactly why you need to dig into your specific state's rulebook.
For families here in New Jersey, figuring out these local details can be a real challenge. At NJ Caregiving, we specialize in helping Mercer County residents understand our state's specific Medicaid respite care guidelines, making sure they can access the full amount of support they're entitled to.
Hypothetical Comparison of State Medicaid Respite Programs
The table below gives you a snapshot of how dramatically different two states can be. It’s a clear example of why you can't rely on general information and must find out what the rules are where you live.
| Feature | State A (Flexible Program) | State B (Restrictive Program) |
|---|---|---|
| Hourly Limits | Offers a flexible annual budget of 200 hours that can be used as needed. | Caps services at 8 hours per week, with no rollover for unused time. |
| Provider Choice | Allows self-direction, meaning families can hire a trusted friend or relative to provide care. | Only allows services from state-certified home care agencies, limiting personal choice. |
| Service Settings | Covers in-home care, adult day care, and short-term stays at a respite facility. | Only covers in-home care, providing fewer options for different family situations. |
| Eligibility Rules | Defines "primary caregiver" broadly, recognizing diverse family support structures. | Has a strict definition of "primary caregiver," potentially excluding some family members. |
As you can see, both states offer something called "Medicaid respite care," but the experience for a family in State A versus State B would be completely different. Your access to care, your flexibility, and your choice of who provides that care all depend on the specific rules your state has put in place.
How to Find a Quality Respite Provider

Once your family gets approved for Medicaid respite care, you’re ready for the next crucial step: finding the right provider. This isn't just about scheduling help; it’s about finding someone you can truly trust with your loved one's well-being. Making a confident, informed choice is what allows you to finally take that deep breath and recharge.
First things first, you need to understand that providers come in a couple of different forms. The options available to you will depend on your state's specific program, but they generally fall into two main buckets.
Agency Professionals vs. Self-Directed Care
Many families choose to work with a state-certified home care agency. These organizations handle all the heavy lifting—they employ professional caregivers who are already vetted, trained, and insured. Going this route provides a great sense of security, since the agency manages the background checks, payroll, and scheduling for you.
On the other hand, many states now offer self-directed (or consumer-directed) programs. This model gives you more flexibility by allowing you to hire someone you already know and trust. It could be a close friend, a neighbor, or even another family member (though rules on which relatives qualify can vary by state). With this option, you essentially become the employer, and Medicaid provides the funds to pay your chosen caregiver. It’s a way to truly personalize the care experience, which can be a huge comfort for everyone involved.
No matter which path you take, the goal is always the same: find a reliable, compassionate, and skilled person who clicks with your family’s needs and personality. The right provider makes all the difference.
Questions to Ask a Potential Respite Provider
Before you make a final decision, it’s essential to sit down for a real conversation. Think of it less like a formal interview and more like a chat to see if it’s a good fit. Having a list of questions ready will help you cover all your bases and compare different people or agencies.
Here is a practical checklist to guide your discussion:
- Experience and Training: What kind of training do you have? Are you experienced in caring for someone with [mention your loved one’s specific condition, like dementia or mobility issues]?
- Handling Challenges: How do you respond if my loved one gets upset or refuses care? Could you share an example of a tough situation you've handled before?
- Emergency Preparedness: What’s your plan for a medical emergency? Are you certified in CPR and First Aid?
- Activities and Engagement: What kinds of activities do you enjoy doing to help someone feel comfortable and engaged?
- Communication Style: How will you keep me in the loop while you're here? Do you prefer to text, call, or keep a written log?
Key Resources for Your Provider Search
The good news is you don't have to do this all on your own. Several organizations are out there specifically to connect families with qualified caregivers. A fantastic place to start is your local Area Agency on Aging (AAA). They have an incredible depth of knowledge about local resources and can give you lists of vetted providers right in your county.
Another great tool is the ARCH National Respite Locator Service. This website helps you find respite programs near you, making it much easier to pinpoint reputable options. For families here in Mercer County, NJ, organizations like NJ Caregiving can simplify the entire process by connecting you directly with skilled, compassionate professionals who specialize in Medicaid respite care.
Your Top Questions About Medicaid Respite Care, Answered
Even after you get the hang of what respite care is, the real-world questions always start to bubble up. You’re probably wondering about the nitty-gritty details, like how many hours you actually get, who can provide the care, and what on earth you’re supposed to do if you run out of support.
Let’s get straight to the point. This section tackles the most common questions caregivers ask, giving you direct answers so you can plan with confidence. Knowing these details helps you manage your respite benefit effectively, ensuring you can take those much-needed breaks without hitting any surprise hurdles.
How Many Respite Hours Can I Get?
This is the big one, but the honest answer is: it depends. There's no single, nationwide standard for the number of respite hours you can receive. The amount varies wildly from one state to the next and even between different Medicaid waiver programs within the same state.
Some states might offer a set number of hours each week, while others provide a more flexible annual allowance of hours or even a dollar amount you can spend.
The exact amount of Medicaid respite care you’re approved for is figured out during your personal needs assessment. A case manager will look at the kind of care your loved one needs, how involved you are as the primary caregiver, and your family's overall situation to determine what's appropriate.
Your best bet is to always check the specific rules for your state's Home and Community-Based Services (HCBS) waiver to see what the limits are.
Can a Family Member Get Paid to Provide Care?
Yes, in many cases, this is absolutely an option! It’s a popular choice offered through what are often called "self-directed" or "consumer-directed" programs. These programs are designed to give families more control and flexibility over their loved one's care.
Basically, you get to hire, train, and manage the caregivers yourself. This often includes family members, though most states have rules preventing spouses or legal guardians from being the paid caregiver. The specific policies on which relatives qualify and how much they can be paid are set by each state, so you'll need to check the details for your local program.
What Happens if I Use All My Allotted Respite Hours?
This is why planning is so important. Once you’ve used up your full allocation of Medicaid-funded hours for the benefit period (which could be a month, a quarter, or a year), you generally have to wait for the next period to start before they renew.
If you run out early, you'll need to find other ways to get a break. Some alternative solutions might include:
- Paying for a private caregiver out-of-pocket.
- Applying for grants from non-profit organizations that support family caregivers.
- Leaning on other family members or trusted friends for support.
Thinking ahead is key to making sure you have coverage when you need it. It's smart to be strategic with your hours, saving them for times when you're feeling particularly stressed or have important appointments you can't miss.
At NJ Caregiving, we help families in Mercer County, including Princeton and Hamilton, understand and access their Medicaid benefits. If you need guidance on navigating respite care, contact us to see how our compassionate team can support you. Learn more at https://njcaregiving.com.


