Preventing pressure ulcers, or bedsores as many call them, really comes down to being proactive and consistent. It's about creating a simple but dedicated routine built on four key actions: regularly repositioning your loved one, checking their skin daily, making sure they're getting good nutrition and hydration, and encouraging safe movement whenever possible. Getting these things right is truly your best defense against these painful and entirely preventable wounds.
A Caregiver's Guide to Pressure Ulcer Prevention
Pressure ulcers are more than just a medical issue; they're a serious threat to an older person's health, comfort, and sense of dignity. These painful sores pop up when constant pressure on one spot—like a heel or hip—cuts off blood flow, causing the skin and tissue underneath to break down. For those of us in a caregiving role, knowing how to prevent pressure ulcers in elderly loved ones isn't just about ticking boxes on a list. It's about developing a mindset of constant watchfulness and compassionate care.
This is a much bigger problem than most people realize. One global study found that the overall incidence of pressure ulcers for people in hospitals is 12%. That number really highlights how critical prevention is, especially for older adults. Beyond the pain and suffering, the financial cost is staggering, with the U.S. healthcare system spending around $11 billion every year to treat them. You can read the full research about pressure ulcer incidence if you want to dig deeper into the scope of the problem.
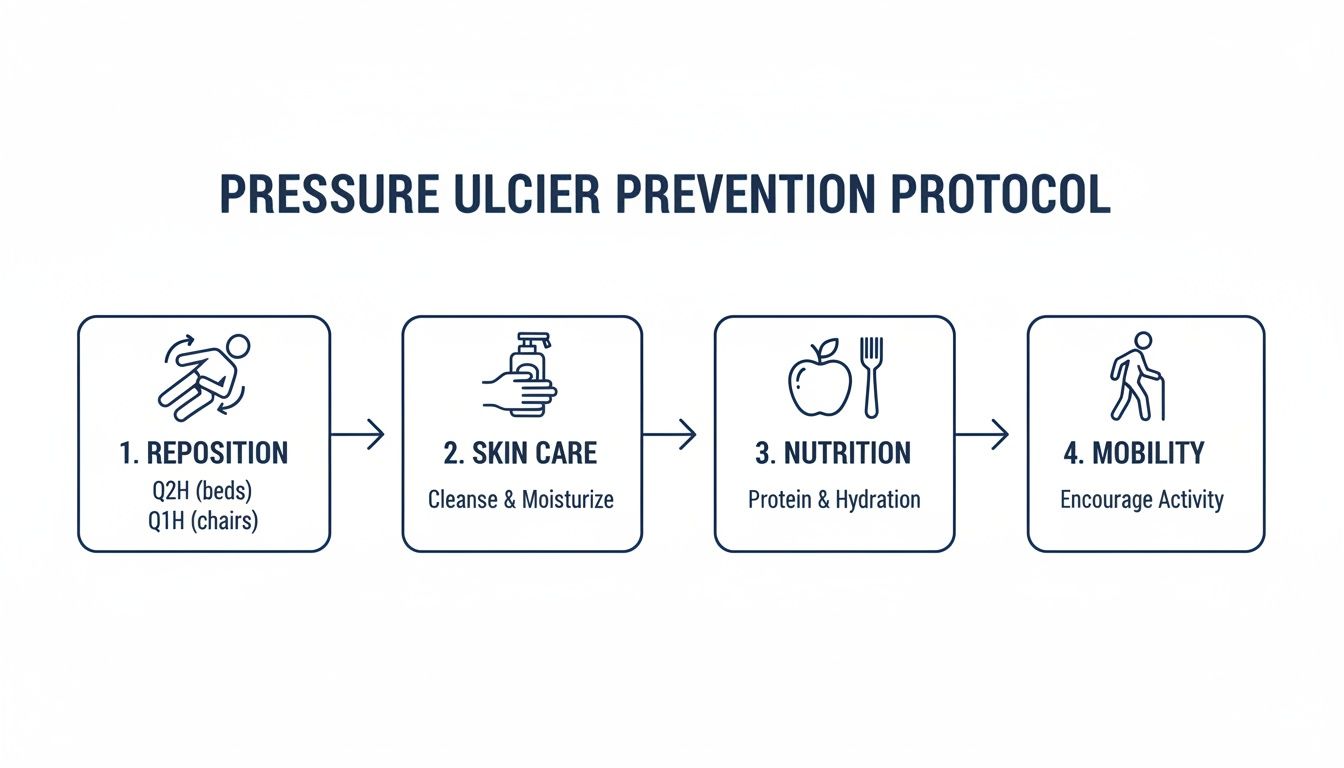
The Four Pillars of Prevention
Your prevention plan is going to stand on four strong pillars. Each one is just as important as the next, and they all work together to protect vulnerable skin.
- Repositioning and Support: This is the big one. Simply shifting weight off bony areas like the hips, tailbone, and heels is the single most effective thing you can do.
- Skin Care and Inspection: A quick daily check for any redness, warmth, or changes in skin texture can help you spot trouble long before it becomes an open wound.
- Nutrition and Hydration: Healthy skin is strong skin. When your loved one is well-nourished and hydrated, their skin is more elastic and resilient against injury.
- Mobility and Exercise: Even small movements make a huge difference. Getting the blood flowing is essential for delivering oxygen and nutrients to the skin.
By focusing on these four pillars, you create a powerful, multi-layered defense. It’s a practical approach that transforms a daunting task into manageable, daily actions that protect your loved one.
Of course, it's also important to stay aligned with professional standards. For the most current, evidence-based practices, I always recommend consulting the latest NPIAP Guidelines. They are the go-to resource for best practices in pressure ulcer prevention.
Key Prevention Strategies at a Glance
To make this even easier to digest, here’s a quick summary of the core strategies. Think of this as your daily checklist for keeping your loved one's skin healthy and intact.
| Prevention Strategy | Why It's Critical | Your First Action Step |
|---|---|---|
| Consistent Repositioning | Relieves constant pressure on bony areas, which is the primary cause of skin breakdown. | Set a timer to help your loved one change position at least every two hours in bed or every hour in a chair. |
| Daily Skin Checks | Allows for early detection of "hot spots" (redness, warmth, firmness) before the skin breaks. | Make a skin check part of the daily routine, like during bathing or dressing. Pay close attention to heels, hips, and the tailbone. |
| Proper Nutrition & Hydration | Well-nourished skin is stronger, heals faster, and is more resistant to injury. | Ensure meals are rich in protein and offer water or other healthy fluids throughout the day. |
| Mobility & Movement | Improves circulation, delivering vital oxygen and nutrients to the skin to keep it healthy. | Even small movements count. Encourage gentle range-of-motion exercises or short walks if possible. |
Wrapping your head around these four areas is the foundation of a successful prevention plan. It’s about turning these concepts into consistent, daily habits.
Mastering Repositioning and Support Surfaces
We’ve all heard the old advice to “turn them every two hours.” It’s a decent starting point, but it barely scratches the surface of what effective pressure ulcer prevention really looks like. True mastery is about understanding the why behind every little shift and choosing the right tools to support your loved one. It’s about being proactive, making thoughtful adjustments that relieve pressure before the damage even has a chance to start.
This focused approach is one of the most powerful ways to protect an elderly person's skin, but challenges definitely remain. Even with modern medicine, pressure ulcer rates in long-term care facilities still hover around 8.6%. Back in 2004, an estimated 159,000 U.S. nursing home residents were suffering from them. These numbers are a stark reminder that consistent, high-quality repositioning isn't optional—it's an absolute necessity.
The Art of the Repositioning Schedule
A fixed two-hour schedule should be treated as a baseline, not a rule set in stone. The ideal frequency really depends on the individual. Someone with very fragile skin or multiple health issues might need small shifts every 30-60 minutes to keep vulnerable areas safe.
And it's not always about a full turn from back to side. Think in smaller, more sustainable adjustments. This is especially important for preserving comfort and letting them get some uninterrupted sleep.
- The 30-Degree Tilt: This is a game-changer. Just a slight tilt to one side, propped up with pillows, can take all the direct pressure off the tailbone without needing a major maneuver.
- Pillow Bridging: Use pillows to "bridge" or lift heels and elbows completely off the mattress. It’s a simple trick that totally eliminates pressure on these incredibly high-risk spots.
- Head of Bed Elevation: If the head of the bed needs to be raised, try to keep it at 30 degrees or less. Anything higher significantly increases the shearing force on their lower back and tailbone.
These small, strategic moves are often more manageable for both of you and just as effective as big, disruptive repositioning efforts. Our guide on safe patient handling techniques dives deeper into how to do these shifts without causing strain.
As you can see, repositioning is the first critical step, but it works hand-in-hand with good skin care, nutrition, and mobility to create a complete protective shield.
Choosing the Right Support Surface
The surface your loved one sits or lies on is just as important as how often they move. The whole point of a support surface is to spread their body weight over a larger area, which dials down the intense pressure on bony spots like the hips, heels, and tailbone. You don't always need a fancy hospital bed, but you do need the right tool for the job.
For example, a standard mattress might be perfectly fine for someone at low risk, but a person who is mostly bed-bound needs something more specialized.
A common mistake I see is people using those donut-shaped cushions. They seem like a good idea, but they can actually cut off blood flow around the very area you’re trying to protect, making the problem much worse.
Key Support Surface Options
- Pressure-Relief Mattresses: These come in a few varieties, from high-density foam to alternating air pressure systems that automatically shift pressure points for you.
- Mattress Overlays: A more budget-friendly option, these are pads made of foam, gel, or air that you place right on top of a standard mattress to improve pressure distribution.
- Wheelchair Cushions: If your loved one spends a lot of time in a chair, a specialized gel, foam, or air cushion is non-negotiable for protecting their tailbone and hips.
- Heel Protectors: These look like soft "boots" and are designed to completely float the heel, getting rid of all pressure on that sensitive area.
For even better repositioning and comfort, it's worth looking into adjustable beds for seniors. When you pair a quality support surface with a diligent repositioning schedule, you create a powerful defense that gives you peace of mind and keeps your loved one’s skin healthy and intact.
A Practical Guide to Daily Skin Care
Beyond simply repositioning, your daily skin care routine is one of the most powerful tools you have to prevent pressure ulcers. It’s all about becoming a detective—learning to spot the subtle clues skin gives you long before a serious problem takes hold.
Consistent, gentle care can make an incredible difference, turning vulnerable skin into a more resilient barrier against injury.

Think of it this way: a small, reddish spot today could become a deep, painful wound in a matter of days if it’s ignored. Daily inspection turns a reactive problem into a proactive solution.
Mastering the Daily Skin Inspection
The best time to check the skin is during routine activities like bathing or dressing. This makes the whole process feel natural and less like a clinical exam. Remember, you're not just looking for open sores; the earliest signs are far more subtle.
Use good lighting and check their entire body, paying extra close attention to bony areas. These "hot spots" are where pressure ulcers are most likely to form first.
- Hips and Tailbone: These are the most common sites for people who spend a lot of time sitting or lying down.
- Heels and Ankles: These spots have very little natural padding, which makes them extremely vulnerable to pressure.
- Shoulder Blades, Elbows, and the Back of the Head: Any point of contact with a bed or chair is a potential risk area.
When you inspect these areas, you need to both look and feel for specific changes. Don't rush it—taking your time to be thorough is key.
A crucial test for a potential Stage 1 pressure injury is the "blanch test." Gently press on a reddened area of skin for a few seconds. If the spot turns white and then red again after you let go, blood flow is still good. If it stays red and doesn't blanch, it's a major warning sign that tissue damage has begun.
What to Look For and Feel For
Your hands can often detect problems just as well as your eyes. As you check each area, run your hand gently over the skin to feel for any changes in temperature or texture.
| Visual Clues to Look For | Tactile Clues to Feel For |
|---|---|
| Redness that doesn't fade (especially in lighter skin tones) | Areas that feel unusually warm or cool to the touch |
| Darker patches that look purple or blue (in darker skin tones) | Skin that feels firmer or softer than the surrounding tissue |
| Swelling, shiny skin, or dry, flaky patches | Any tenderness or pain reported by your loved one |
| Blisters, cracks, or any break in the skin | Bogginess or a mushy feel under the skin |
If you're caring for someone with dementia, they might not be able to tell you they're in pain. In these situations, your daily visual and touch checks become even more critical. Watch for non-verbal cues like wincing or pulling away when you touch a sensitive spot.
Gentle Cleansing and Moisture Management
Healthy skin is clean and properly moisturized, but harsh soaps and aggressive scrubbing can do more harm than good. The goal here is to be gentle. Use a mild, pH-balanced cleanser and warm (not hot) water.
Always pat the skin dry with a soft towel. Never rub, as this creates friction that can easily damage fragile skin.
Moisture can be a double-edged sword. While dry, cracked skin is weak, skin that is constantly damp from sweat or incontinence is also at high risk for breakdown.
After cleansing, apply a high-quality moisturizer to their entire body to lock in hydration. If incontinence is an issue, a barrier cream is absolutely essential. These products create a protective seal, shielding the skin from the irritating effects of urine and feces. This simple step is a non-negotiable part of how to prevent pressure ulcers in elderly individuals who need help with toileting.
The Role of Nutrition and Hydration in Skin Health
What you serve on the plate has a direct and powerful impact on your loved one's skin health and its ability to resist breakdown. Think of good nutrition as building a stronger, more resilient shield from the inside out. When the body has the right building blocks, skin becomes tougher, more elastic, and better equipped to handle the constant threat of pressure.
This isn't just about eating enough; it's about eating the right things. A balanced diet provides the essential vitamins, minerals, and proteins needed for continuous skin repair. Without these nutrients, the skin weakens, becoming fragile and far more susceptible to injury.
The Powerhouse Nutrients for Skin Resilience
Certain nutrients are absolute superstars when it comes to skin integrity. As a caregiver, focusing on these in daily meals is one of the most practical and effective ways to bolster their defenses against pressure sores.
- Protein: This is the undisputed champion. Protein is essential for building and repairing all body tissues, including the skin. Without enough, the body can't heal minor damage, which can quickly escalate into a full-blown pressure ulcer.
- Vitamin C: Think of Vitamin C as the mortar holding the skin's bricks together. It’s vital for producing collagen, the protein that gives skin its strength and elasticity.
- Zinc: This mineral is a key player in wound healing and immune function. A zinc deficiency can dramatically slow down the body's ability to repair skin damage.
The link between poor nutrition and pressure ulcers is undeniable. In U.S. nursing homes, a staggering 20% of residents who have recently lost weight develop ulcers, compared to just 10% of those who haven't. This makes nutritional support a cornerstone of prevention, especially for seniors dealing with other risk factors. Focusing on diet is a key part of managing the $11 billion spent annually in the U.S. on this preventable condition. You can discover more insights about these risk factors at Fortune Business Insights.
Overcoming Common Eating Challenges in Seniors
Knowing what nutrients are important is one thing, but getting an elderly person with a poor appetite to eat them is another challenge entirely. Many seniors struggle with a decreased sense of taste, difficulty chewing, or just a general lack of interest in food.
The key is to make every single bite count.
It's not about forcing large meals. Instead, think about offering smaller, more frequent meals and snacks throughout the day. A nutrient-rich smoothie can be far more appealing—and effective—than a large plate of food they won't touch.
Practical Meal and Snack Ideas
Getting these critical nutrients into a senior's diet doesn't have to be complicated. Here’s a quick look at some easy, skin-boosting foods you can incorporate. For more ideas, be sure to check out our complete guide on nutrition tips for elderly individuals.
The table below breaks down some simple, senior-friendly food sources for those key nutrients.
Skin-Boosting Foods for Senior Diets
| Nutrient | Role in Skin Health | Easy-to-Eat Food Sources |
|---|---|---|
| Protein | Essential for tissue building, repair, and overall strength. | Scrambled eggs, Greek yogurt, cottage cheese, protein shakes, smooth peanut butter, flaked fish. |
| Vitamin C | Crucial for collagen synthesis, which gives skin its structure. | Orange juice, strawberries, bell pepper strips, tomato soup, mashed sweet potatoes. |
| Zinc | Supports immune function and is vital for wound healing. | Fortified cereals, cooked spinach, beans, ground beef, yogurt. |
Focusing on these types of foods can turn mealtime into a powerful prevention tool, helping to fortify the skin from within.
Hydration Is Not Negotiable
Finally, we can't talk about nutrition without emphasizing hydration. Dehydrated skin loses its elasticity, making it papery, brittle, and much more prone to tearing under pressure. It's like a dry, brittle leaf compared to a fresh, flexible one.
Many older adults don't feel thirsty, so you can't rely on them to ask for a drink. You have to be proactive.
- Offer Fluids Frequently: Keep a water bottle or a favorite beverage within easy reach at all times.
- Think Beyond Water: Soups, broths, gelatin, and water-rich fruits like melon and oranges all contribute to their daily fluid intake.
- Set a Schedule: Make offering a drink a regular part of your routine—when they wake up, with medications, and between meals.
By making nutrition and hydration a central pillar of your care plan, you give your loved one’s body the internal resources it needs to maintain healthy, resilient skin.
Encouraging Safe Movement and Mobility
There’s an old saying: "an object in motion stays in motion." This couldn't be more true when it comes to preventing pressure ulcers. For our elderly loved ones, even the smallest movements can make a world of difference for their skin health by boosting blood flow and relieving constant pressure. The goal isn’t to run a marathon; it’s about thoughtfully integrating safe, practical mobility into the daily routine.

When someone stays in one spot for too long, blood flow gets cut off, starving the skin tissue of the oxygen it needs to survive. Movement, even gentle exercises from a bed or chair, directly counters this by getting the circulation going again. It’s a simple idea with a powerful protective effect.
Simple Exercises from a Bed or Chair
For seniors with limited mobility, their bed or a favorite chair can become a personal gym. The following exercises don't require any special equipment and are designed to improve circulation, especially in the legs, where pressure sores often pop up on heels and ankles.
- Ankle Pumps: While lying down or sitting, have them slowly point their toes away from their body, then pull them back up toward their shins. Aim for 10-15 repetitions every hour or two. This simple motion acts like a pump for the calf muscles, helping push blood back up the legs.
- Ankle Rotations: Ask them to gently rotate their feet in clockwise circles, then switch directions. This helps with joint flexibility and gets blood moving all around the foot and ankle.
- Leg Lifts: If they're able, have them sit up and slowly extend one leg straight out, hold it for a few seconds, and then gently lower it back down. This strengthens the thigh muscles and boosts circulation through the entire leg.
The key here is consistency, not intensity. A few minutes of gentle movement several times a day is far more beneficial than one strenuous, exhausting session.
For a more detailed list of safe movements, our guide on leg exercises in bed has more easy-to-follow suggestions you can weave into your daily care routine.
Promoting Safe Walking and Transfers
If your loved one can still walk, even with help, encouraging this activity is one of the best things you can do. Walking is a full-body exercise that dramatically improves circulation, maintains muscle tone, and gives a significant mental health boost.
Of course, safety always comes first. Make sure they are using any prescribed assistive devices correctly, whether it’s a walker or a cane. The walking path should be clear of hazards like throw rugs or clutter that could easily cause a fall.
Even short walks—from the bedroom to the kitchen or a few trips down the hallway—can make a huge difference in reducing pressure sore risk. The simple act of standing up and bearing weight shifts pressure off the very areas most at risk when sitting or lying down.
Passive Range of Motion for Limited Mobility
For individuals who are completely bed-bound and can't move on their own, you can still help their bodies stay mobile through passive range-of-motion (PROM) exercises. This is where you, as the caregiver, gently move their joints for them.
The idea is to carefully support a limb, like an arm or leg, and move it through its natural range of motion. For instance, you would gently bend and straighten their knee or move their arm in slow, controlled circles.
- Support the Joint: Always place one hand above and one hand below the joint you are moving.
- Move Slowly and Gently: Never force a movement or push past a point of resistance or pain. The motion should be smooth and easy.
- Be Comprehensive: Try to work through all major joints, including the shoulders, elbows, wrists, hips, knees, and ankles.
These exercises are crucial for preventing stiff joints and shortened muscles, but they also stimulate blood flow to tissues that would otherwise be stagnant. By integrating these small but meaningful movements into your daily routine, you empower your loved one's body to better defend itself against the constant threat of pressure ulcers.
When to Seek Professional Support
Even with the most dedicated effort, there are times when the complexities of caregiving just require professional support. Knowing when to raise your hand and ask for help isn't a sign of failure—it’s the mark of a smart, proactive caregiver who is committed to providing the absolute best care for their loved one.
You've learned how to reposition, check skin, and encourage nutrition, but sometimes, a situation simply calls for an experienced team.
Recognizing the early warning signs is everything. If you notice a reddened area that doesn't fade, a small blister, or any kind of break in the skin, it’s time to act immediately. These initial stages can progress alarmingly fast. Getting a professional involved can stop a minor issue from turning into a serious, painful wound.
Clear Signs You Need to Call for Help
Don't wait for the situation to get worse. You should seek professional support if you observe any of the following, because early intervention is truly the key to preventing a severe pressure injury.
- A Non-Blanching Red Spot: This is a major red flag. If you press on a red area and it doesn't briefly turn white, this is a Stage 1 pressure injury.
- Any Break in the Skin: This includes blisters, scrapes, or shallow craters. It's a sign the wound has already progressed to Stage 2.
- Signs of Infection: Increased pain, a foul odor coming from the wound, pus-like drainage, or warmth and swelling around the area all demand immediate medical attention.
- Rapid Decline in Health: If your loved one suddenly becomes less mobile, stops eating, or seems unusually tired, their risk for skin breakdown skyrockets.
How Professional Home Care Makes a Difference
This is exactly where a service like NJ Caregiving can provide critical support. Bringing in professional caregivers doesn't mean you're stepping away. Think of it as adding an expert layer to your loved one’s defense system. A home care agency provides a structured, experienced approach to prevention that can be hard to maintain on your own.
For instance, a registered nurse can conduct a formal risk assessment and create a personalized care plan that addresses your loved one's specific needs. Trained caregivers then execute this plan with precision, ensuring repositioning schedules are followed to the letter and skin checks are performed with a clinical eye. This support also provides essential respite for family caregivers, helping to prevent the burnout that makes consistent care so challenging.
Think about this real-world scenario: An 85-year-old man in Mercer County is recovering from pneumonia and is extremely weak. His daughter is doing her best, but he resists being moved and has a poor appetite. A professional caregiver can use specialized techniques to make repositioning more comfortable and work with the family to introduce nutrient-dense supplements, stopping a potential pressure ulcer before it even has a chance to start.
Ultimately, preventing pressure ulcers is a team effort. Recognizing your own limits and partnering with professionals ensures your loved one receives the comprehensive, consistent care they need to stay safe, healthy, and comfortable at home.
Your Questions, Answered
Even with the best plan, you're bound to have questions as you handle the day-to-day realities of caregiving. We get it. Here are some of the most common things families ask us when they’re working to prevent pressure ulcers.
How Often Should I Reposition My Elderly Parent?
That classic "every two hours" advice is a great starting point, but it’s not a one-size-fits-all rule. The truth is, the right timing really depends on the individual.
If your parent has very fragile skin or other health issues, small shifts every 15 to 30 minutes while they're awake can make a huge difference. And don't think you need to do a full-body turn every time. Simply using a pillow to lift their heels completely off the mattress or slightly shifting their weight off one hip counts. A visiting nurse or physical therapist can be a fantastic resource for creating a personalized schedule that works for everyone.
Is an Expensive Mattress Really Necessary?
Not always, but having the right surface to lie on is absolutely critical.
For someone at high risk—maybe they're mostly bed-bound or have had skin issues before—a pressure-redistribution mattress is often a game-changer. These specialized surfaces are designed to spread out pressure and can be well worth the investment. For those at lower risk, you can often get by with high-density foam overlays or specialized cushions for their wheelchair, as long as you’re consistent with repositioning. It’s all about matching the equipment to their specific level of risk and mobility.
No mattress, no matter how advanced, can ever replace a consistent repositioning schedule. The surface is just a tool; your consistent care is what truly prevents these sores.
What Are the First Signs of a Pressure Ulcer?
The earliest warning sign isn’t what most people expect. A Stage 1 pressure injury isn't an open wound at all.
Instead, you’ll see a patch of skin that stays red even after you press on it (the medical term is non-blanching redness). It usually appears over a bony spot like the tailbone, hips, or heels. That area might also feel different—warmer, cooler, firmer, or softer than the skin around it. Sometimes, your loved one might complain about pain or itching in that spot. Spotting these signs is your best chance to act fast and stop it from getting worse.
Trying to manage all the details of pressure ulcer prevention can feel like a lot to handle, but you’re not in this by yourself. The compassionate team at NJ Caregiving is here to offer expert support, from skilled nursing assessments to hands-on help with daily skin care and repositioning. Visit our website at https://njcaregiving.com to see how we can help you protect your loved one’s health and give you peace of mind.


