A home health care assessment form is the absolute cornerstone of any safe, effective, and truly personal in-home care plan. It’s so much more than just paperwork; it’s the detailed blueprint that captures a client's complete medical, functional, and environmental needs. Think of it as the primary tool for shaping high-quality care from day one.
The Foundation of Personalized Home Care

This form is your agency's first, best chance to understand a new client—not just as a patient, but as a person with unique routines, preferences, and potential risks. It's the starting point of a crucial conversation, the one where you gather the critical insights that will drive every single care decision you make moving forward.
This isn’t about just ticking off boxes on a checklist. A well-designed assessment guides a structured yet empathetic discovery process. It makes sure nothing critical gets missed, from complex medication schedules to something as simple as the height of a shower ledge.
More Than Just Paperwork
From a practical standpoint, this single document accomplishes several key goals at once. It serves as a vital legal and regulatory safeguard, showing your agency’s diligence and adherence to professional standards. Frankly, a thorough assessment process directly elevates your standard of care and sets you apart in a competitive market.
Getting this right is becoming more important every day. The global home healthcare market, valued at around USD 416.4 billion, is projected to nearly double by 2030. A big reason for this growth is the proven effectiveness of in-home programs, which can reduce care costs by over 30% compared to long hospital stays. You can explore more about these industry trends and what they mean for your agency.
A great assessment tells a story. It paints a detailed picture of the client's world, allowing your team to step in with support that is not just helpful, but genuinely empowering.
Core Components of a Home Health Assessment Form
To build a care plan that actually works in the real world, your assessment has to be structured around several key areas. Each section logically builds on the last, creating a holistic profile of the client’s situation. Understanding these components is the first step to mastering the assessment process.
Here’s a quick overview of the essential sections you’ll find in a comprehensive home health assessment and the primary purpose behind each one.
Core Components of a Home Health Assessment Form
| Section | Primary Purpose |
|---|---|
| Client Intake & Demographics | Gathers basic personal, contact, and insurance information. |
| Medical History | Documents diagnoses, allergies, medications, and recent hospitalizations. |
| Functional Status (ADLs/IADLs) | Assesses ability to perform daily self-care and household tasks. |
| Risk & Safety Assessment | Identifies potential hazards in the home environment. |
| Care Plan Goals | Defines client-centered objectives for the care period. |
With these pieces in place, you have everything you need to move from assessment to action, crafting a plan that truly meets the needs of the individual you're serving.
Navigating Client Intake and Medical History
That first conversation with a new client is where everything starts. It’s so much more than just ticking boxes on a home health care assessment form. This is your chance to build trust and show you’re there to listen, all while gathering the critical information you need to provide safe, personalized care. We’re moving beyond just names and insurance info into the heart of their medical story.
Think of this part of the process as laying the foundation for a house. If that foundation is shaky—if you miss a key piece of their health history—the entire care plan you build on top of it could have serious problems. We've seen it happen. Small oversights at this stage can lead to major issues later, from medication mix-ups to using the wrong care techniques. Getting this right from day one is non-negotiable.
Capturing the Full Medical Picture
When you're documenting a client's medical history, your mission is to see the whole person, not just their primary diagnosis. It’s easy to focus on the main reason they need care, but the other conditions—the comorbidities—are just as important. For instance, a client whose main issue is heart failure might also be dealing with diabetes and peripheral neuropathy. Suddenly, you're not just managing cardiac symptoms; you're also thinking about mobility challenges and specialized wound care.
To make sure nothing slips through the cracks, it helps to have a system. We always make sure our intake process covers:
- Allergies: Go beyond just asking if they have allergies. Ask what happens when they're exposed. Document every known allergy—medications, foods, environmental triggers—and the specific reaction.
- Current Medications: Get a complete list of everything. That means all prescriptions, any over-the-counter drugs, and even vitamins or supplements. For each one, you need the dose, how often they take it, and why.
- Recent Hospitalizations: Any hospital or rehab stays in the last 6 to 12 months are relevant. Find out why they were admitted and what the discharge summary said. This gives you a snapshot of recent acute events.
- Chronic Illnesses: List every ongoing condition. Think COPD, kidney disease, arthritis, dementia—anything that’s a long-term part of their health landscape.
Key Takeaway: A detailed medical history isn't just a best practice; it's a must for regulatory compliance. It's the information the certifying physician relies on and what ensures your care plan addresses every related condition, a core requirement under Medicare guidelines.
Asking the Right Questions
How you ask for this information matters just as much as what you ask. Firing off a list of yes-or-no questions can feel like an interrogation and won't get you the rich details you really need. The key is to use open-ended prompts that get them talking.
Here’s what I mean:
- Instead of, "Are you in pain?" you could try, "Tell me about any discomfort you feel throughout the day."
- Instead of, "Do you take your medicine?" ask, "Can you walk me through your typical morning routine for taking your medications?"
This conversational style helps you uncover the client's lived experience. You might learn that they struggle to open pill bottles or that they sometimes forget a dose—practical challenges that are goldmines for building a truly effective care plan.
Don't forget to involve family members, especially if your client has memory or cognitive issues. They can often fill in the gaps and provide a more complete picture. The goal here is a team effort that respects the client’s dignity while making sure every detail is accurate.
A Practical Guide to ADL and IADL Evaluation

This part of your home health care assessment form is where the rubber meets the road. It's where you move past the medical chart and discover how a client actually navigates their day-to-day world. This involves looking closely at two key areas: Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs).
Think of it this way: ADLs are the absolute basics of self-care, while IADLs are the more complex tasks required to live independently in the community.
Getting this right is crucial for building a care plan that provides just the right amount of support without taking away a client's independence. The image above gives a fantastic visual breakdown. You'll see ADLs are about personal care like bathing and eating, whereas IADLs cover things like managing finances or getting to appointments.
Assessing Activities of Daily Living (ADLs)
ADLs represent the most fundamental self-care skills. When you're evaluating these, your goal is to pinpoint where hands-on help is genuinely needed versus where a client can manage on their own, perhaps with a little encouragement or standby assistance.
The best way to get accurate information is through observation and friendly conversation, not a clinical-feeling interrogation. For instance, instead of a blunt "Can you bathe yourself?", try a gentler approach: "Tell me a little about how you manage getting in and out of the shower. Do you have any worries about that?" This opens the door to a much more detailed and honest conversation.
Here are the key ADLs to look at:
- Bathing and Grooming: Can they safely get into the shower or tub? Are they managing personal hygiene like brushing their teeth or combing their hair without issues?
- Dressing: Notice if they struggle with buttons, zippers, or even putting on socks and shoes. Sometimes the clothing itself tells a story—is it appropriate for the weather?
- Toileting: Can they get to the bathroom and back on their own? Do they need any help with cleanup? This is often a sensitive subject, so always approach it with compassion and professionalism.
- Transferring and Mobility: Simply watch how they move. How do they get up from a chair? Do they use a walker or cane? Do they grab onto furniture for support as they walk across the room?
- Eating: This isn't about their cooking ability, but the physical act of eating. Note if they have trouble using utensils, bringing food to their mouth, or swallowing.
Evaluating Instrumental Activities of Daily Living (IADLs)
IADLs are a step up in complexity, demanding more planning and cognitive skill. A decline here is often one of the first signs that more support is needed, even if a client seems to be handling their basic ADLs just fine. You can see how these are often laid out by looking at this sample home care plan from NJ Caregiving.
A classic example I’ve seen countless times: a client proudly says they handle their own medications. But when you ask to see their pillbox, it’s a jumbled mess. That single observation is far more telling than their initial answer.
Here’s how you can gently probe into the most common IADLs:
- Medication Management: Ask to see their system. "Can you show me how you keep your pills organized?" Check if they use a weekly dispenser and if they can explain what each medication is for.
- Meal Preparation: A simple "What did you have for lunch yesterday?" can be very revealing. It tells you if they're cooking for themselves or mostly relying on frozen dinners and takeout.
- Housekeeping: Take a look around. Is the home reasonably clean and free of major clutter? Piles of mail, unwashed dishes, or tripping hazards can be red flags for physical or cognitive struggles.
- Managing Finances: Gently ask how they handle paying bills. Are they still writing checks and mailing them, or has a family member stepped in to help?
- Transportation: How do they get groceries or make it to the doctor? Find out if they're still driving, comfortable with public transit, or completely reliant on others.
Ultimately, your goal is to translate all these observations into a clear, realistic picture of your client's needs. This ensures the care plan you create is both respectful of their abilities and effective in keeping them safe.
Creating a Safer Home Environment

For high-quality home care, a safe living space is absolutely non-negotiable. This section of your home health care assessment form is where you’ll conduct a comprehensive home safety evaluation, a crucial step that protects both your client and your caregivers.
This isn't just about ticking boxes to prevent accidents. It’s a proactive measure that shows your agency’s deep commitment to holistic well-being. Getting this right can even help reduce the risk of frustrating and costly hospital readmissions.
A truly thorough risk assessment means methodically inspecting the home for potential dangers. It’s far more than a quick glance around. You need a detailed eye to spot hazards that residents might have gotten used to and no longer even notice. The whole point is to find and fix risks before an incident ever happens.
Pinpointing Common Home Hazards
Your assessment should kick off by looking for the most common culprits behind in-home accidents, particularly falls. Falls are a leading cause of serious injury among older adults, and so many of them are preventable with just a few simple changes.
As you walk through the home, pay close attention to these key areas:
- Floors and Walkways: Keep an eye out for loose area rugs, curled carpet edges, or electrical cords stretched across walking paths. These are some of the most frequent tripping hazards we see.
- Lighting: Is there enough light in hallways, stairwells, and bathrooms? Poorly lit areas make it incredibly difficult to navigate safely, especially in the middle of the night.
- Bathrooms: This is a high-risk zone. Make a note if you don't see grab bars in the shower or near the toilet. Also, check for slippery tub floors or a low toilet seat that makes standing up a real challenge.
- Kitchen: Look for everyday items stored on hard-to-reach high shelves, a lack of clear counter space, and how accessible essential appliances are.
We once had a client whose family couldn't figure out why he kept having minor falls. Our assessment revealed the culprit was a beloved but badly frayed antique rug in his main hallway. Removing it instantly made his home safer.
Specialized Assessments for Unique Needs
A standard checklist is a fantastic starting point, but a truly personalized safety evaluation digs deeper. Your approach has to adapt to the client's specific health conditions and their social situation.
Cognitive Decline and Environmental Safety
When a client has dementia or cognitive decline, their home can present a unique set of challenges. Your assessment needs to look for potential risks tied to memory loss and confusion.
- Are medications stored securely and out of reach?
- Do exterior doors have locks to prevent wandering?
- Are sharp objects or potentially toxic cleaning supplies safely put away?
Evaluating Social and Emotional Risks
Safety isn't just about physical hazards. Social isolation is a huge risk factor for declining health in seniors. As you conduct your assessment, observe for signs that a client might be lonely or disconnected. Is the house unusually quiet? Does the client mention not having many visitors or social outings?
Documenting these observations on the home health care assessment form is vital. It allows you to build companionship and social engagement directly into the care plan, addressing a crucial—and often overlooked—aspect of your client’s well-being.
Translating Assessments into Actionable Care Plans
So you've meticulously completed the home health care assessment form. Now what? The real magic happens when you turn all that information into a living, breathing care plan. This document isn't just a stack of notes; it becomes the single source of truth for your entire team. It takes all the puzzle pieces—medical history, ADL needs, safety risks—and assembles them into a practical guide for every caregiver who walks through the client's door.
A truly great care plan does more than list tasks. It tells a story. It gives clear, confident direction so that every caregiver, whether they're a veteran or new to the case, understands the client’s unique situation and preferences. This synthesis is the foundation for providing consistent, high-quality care and seeing real, positive outcomes for your clients.
Setting SMART Goals Collaboratively
I've learned over the years that the most effective care plans are built with the client and their family, not just for them. When everyone has a seat at the table, you get buy-in. The best way to make this collaboration productive is by setting SMART goals. This simple framework turns vague wishes into concrete, trackable objectives that everyone can get behind.
Here’s how it breaks down in a real-world scenario:
- Specific: Instead of a vague goal like "Improve mobility," get specific. A much better goal is, "Client will walk to the mailbox and back with their walker, with standby assistance, three times per week."
- Measurable: The goal has a clear benchmark for success. Did they do the walk three times this week? Yes or no. It’s easy to track.
- Achievable: This one is crucial. The goal has to be realistic. If a client can barely make it across the living room, aiming for the mailbox right away is setting them up for failure. Start smaller.
- Relevant: Does this goal actually matter to the client? Maybe their main motivation is attending a grandson's birthday party in a month. Frame the mobility goal around building the strength and endurance needed for that special outing. That connection makes all the difference.
- Time-Bound: Put a deadline on it. For example, "We will work toward this goal for the next 30 days and then review our progress."
This collaborative process gives the client a sense of ownership and motivation. When they help create the plan, they're far more engaged in the work it takes to succeed. You can see how these goals directly inform the day-to-day tasks in our guide to effective care planning.
A care plan is more than a to-do list; it’s a dynamic roadmap. It should be reviewed and updated regularly—at least every 60 days or whenever there's a significant change in the client's condition—to ensure it always reflects their current needs and aspirations.
From Goals to Daily Caregiver Tasks
Once your SMART goals are locked in, the next step is to break them down into specific, daily caregiver tasks. This is where your plan gets its legs. It’s also where regulatory compliance comes into sharp focus, especially with today's payment models.
For example, recent Medicare changes have put more pressure on agencies to justify their services. For 2025, CMS projected a small 0.5% payment increase, but that comes with a permanent -1.975% adjustment tied to the Patient-Driven Groupings Model (PDGM). This financial reality means your care plans must be more than just client-centered; they need to demonstrate clear, efficient, and justifiable service delivery. You can read the full CMS fact sheet on these payment updates to get into the nitty-gritty.
Your plan has to clearly outline everything from communication protocols and emergency procedures to the specific actions caregivers will take on each and every visit. This level of detail isn't just about ticking boxes—it ensures consistency, supports your quality assurance efforts, and creates a solid record of the excellent care your agency provides.
Adapting Assessments for Hospital-at-Home Care
The rise of Hospital-at-Home (HaH) programs is one of the biggest changes we've seen in modern healthcare. This isn't just about providing care at home; it's about delivering hospital-level services in a residential setting. And that means your standard home health care assessment form needs a serious upgrade.
When a client is receiving acute care at home, the assessment shifts from a simple safety check to a detailed clinical and logistical review. It's a whole new ballgame.
Focusing on Technical and Emergency Readiness
Your focus needs to sharpen considerably, zeroing in on the home's infrastructure. Can the environment physically and electrically support sophisticated medical equipment? I'm talking about more than just finding a spare outlet. You need to identify stable surfaces for IV poles, check for enough space to operate an oxygen concentrator without it becoming a tripping hazard, and—most importantly—verify the presence of grounded outlets that won't overload. The last thing you want is a fire risk from a cardiac monitor.
Beyond the physical space, digital connectivity is absolutely critical. In HaH models, telehealth appointments and remote patient monitoring are the norm. A spotty Wi-Fi signal isn't just a minor annoyance; it represents a complete breakdown in the care continuum.
The visual below highlights the difference in scope and timing between that intensive first assessment and the more targeted follow-ups.
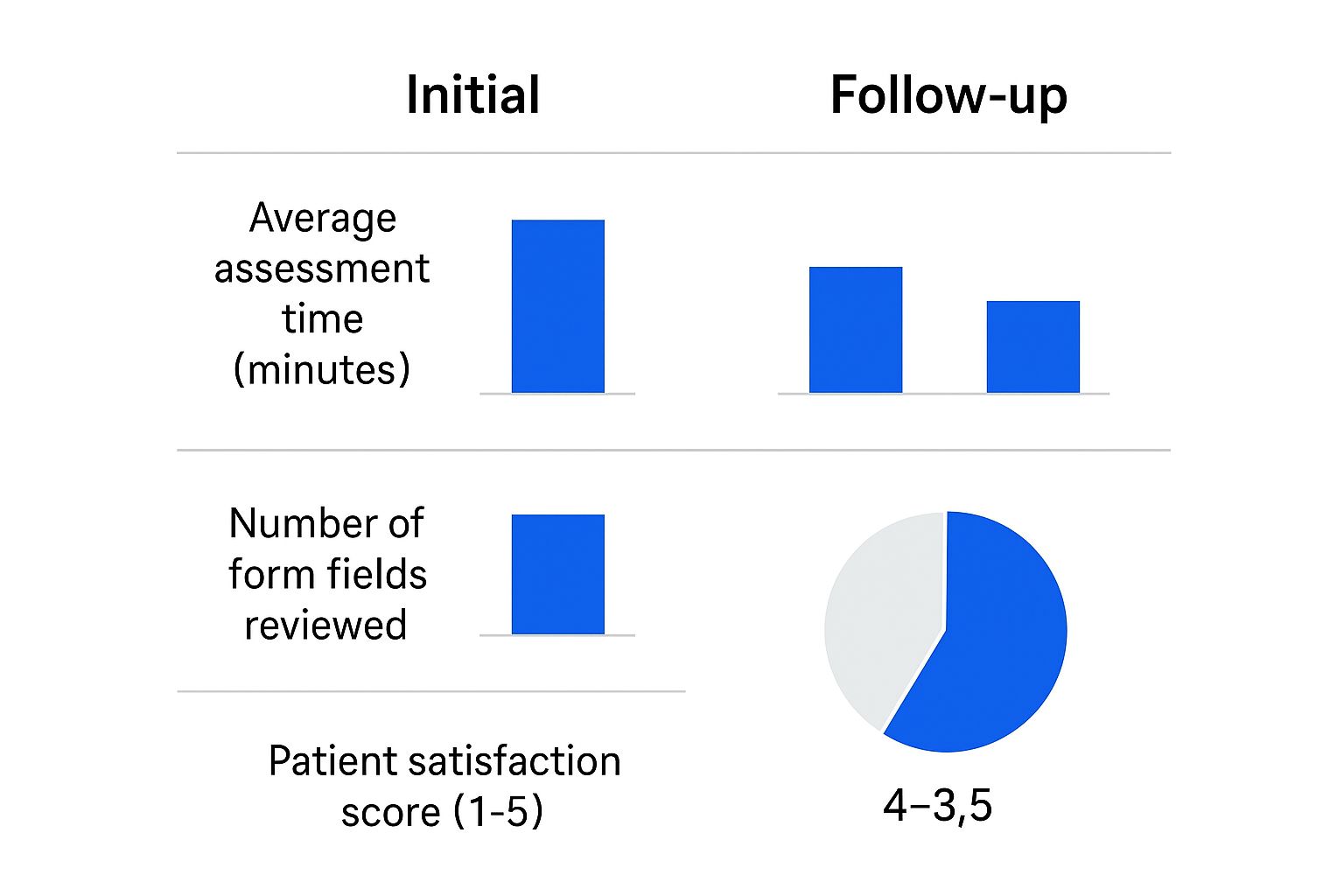
As you can see, a thorough initial assessment paves the way for much more efficient follow-ups, which goes a long way toward keeping patient satisfaction high.
These HaH programs are growing fast. As of 2025, more than 350 hospitals across 37 states are now providing CMS-approved inpatient care at home. This model also makes financial sense, with an average admission cost of around $5,800, which is significantly less than the $7,700 for a traditional hospital stay.
Key Takeaway: For Hospital-at-Home, your assessment isn't just asking, "Is the home safe for daily living?" It must answer the question, "Is this home ready to function as a temporary hospital room?" This requires you to anticipate a much higher level of medical acuity.
The table below breaks down the key differences in focus between a traditional assessment and one designed for a Hospital-at-Home setting.
Traditional vs. Hospital-at-Home Assessment Focus
| Assessment Area | Traditional Home Care Focus | Hospital-at-Home (HaH) Focus |
|---|---|---|
| Environment | General safety, fall risks, accessibility | Electrical capacity, space for medical devices, stable surfaces |
| Technology | Emergency contact system (e.g., life alert) | Reliable high-speed internet, cellular backup, device compatibility |
| Caregiver Role | Assistance with ADLs, companionship | Training on medical equipment alarms, recognizing clinical changes |
| Emergency Plan | Contacting 911, family notification | Specific protocols for equipment failure, rapid response team contact |
This comparison really drives home how much more technical and forward-thinking an HaH assessment needs to be.
Finally, your form must include a much more detailed review of emergency protocols. This includes making sure family caregivers are prepared. They may need hands-on training for responding to equipment alarms or spotting subtle changes in a patient's condition that demand immediate clinical action. Our guide for developing effective home care plans is a great resource for documenting these kinds of advanced protocols.
Getting this specialized HaH assessment right is what will set your agency apart, especially as the industry moves more toward value-based care.
Common Questions About Home Health Assessments
When you're arranging care, it's natural to have questions about the assessment process. Getting the right answers helps everyone feel confident and ensures the care plan truly reflects your loved one's needs. Here are a few things we often discuss with families.
How Often Should a Home Health Assessment Be Updated?
As a general rule, we conduct a full reassessment at least every 60-90 days. Life changes, and so do care needs.
However, we don't just wait for the calendar. It's critical to perform a new assessment anytime there's a significant shift in a client's health. This could be after a hospital stay, a bad fall, or a new medical diagnosis. These regular check-ins make sure the care plan never becomes outdated and continues to provide effective, relevant support.
What Is the Biggest Mistake to Avoid During an Assessment?
The most common pitfall we see is when an assessment is treated like a simple checklist. Rushing through the questions without genuine engagement is a missed opportunity. A quality assessment is really a conversation built on active listening, sharp observation, and building a real connection.
Simply firing off questions isn't enough. The real insights come from the follow-ups. Ignoring the non-verbal cues—like a wince of pain when someone stands up or a moment of hesitation before answering—will always lead to an incomplete and less effective care plan.
Can Family Complete the Assessment Form for the Client?
Family input is incredibly valuable, and we always encourage it. You know your loved one best. However, the assessment must always be centered on the client themselves.
Whenever possible, we gather information directly from the client to honor their autonomy and dignity. If someone is dealing with cognitive challenges, a family member's help is essential. In those cases, the assessor's direct observations are still a vital piece of the puzzle, and we make sure to document this collaborative approach right on the form.
At NJ Caregiving, we believe a detailed and compassionate assessment is the foundation of exceptional in-home care. If you're looking for dedicated, personalized support for a loved one in Mercer County, we invite you to explore our home care services.


