Leaving the hospital can feel like a whirlwind of instructions, medications, and appointments. A smooth transition is crucial for recovery and preventing readmission, but the process is often overwhelming. A structured approach can make all the difference, transforming confusion into confidence and ensuring a safe return home.
This comprehensive discharge planning checklist provides a clear roadmap for you and your family. It breaks down the six most critical areas to address before leaving the hospital, from medication management to home safety. We will move beyond generic advice to offer actionable steps, practical examples, and specific questions to ask your healthcare team.
By following this guide, you will build a strong safety net for post-hospital care. You will learn precisely how to coordinate follow-up appointments, understand new care routines, and connect with necessary community resources. This checklist is designed to empower you with the knowledge needed to manage recovery effectively, reduce the risk of complications, and ensure a secure healing journey. Let's dive into the essential components that will pave the way for a successful transition from hospital to home.
1. Medication Reconciliation and Education
Medication errors are one of the most common and dangerous risks during a hospital-to-home transition. Medication reconciliation is a formal process designed to prevent these errors by creating the single most accurate list of a patient's medications. This crucial step in any comprehensive discharge planning checklist involves a systematic review of all medications the patient was taking before, during, and after their hospital stay.
The primary goal is to identify and resolve discrepancies, such as omissions, duplications, dosing errors, or harmful interactions. This process, often led by a pharmacist or a dedicated nurse, ensures that the final medication list is correct and appropriate for the patient's current health status.
Why It's a Critical First Step
Without meticulous reconciliation, patients can easily become confused. They might continue taking a medication that was discontinued in the hospital or take two different versions of the same drug. These mistakes can lead to adverse drug events (ADEs), hospital readmissions, and serious health complications.
Leading healthcare organizations like The Joint Commission and the Institute for Healthcare Improvement (IHI) have established medication reconciliation as a standard of care precisely because of its high impact on patient safety.
Key Insight: Think of medication reconciliation not just as a task, but as a safety-critical communication tool. It ensures that the patient, their family, the hospital care team, and their primary care physician are all working from the same, accurate medication playbook.
Practical Implementation and Actionable Tips
Successfully integrating this into your discharge plan involves more than just creating a list. It requires clear, patient-centered education.
- Provide a "Pill Card": Create a simple, printed card that lists all medications. Include the brand and generic names, dosage, what it's for, and the time of day it should be taken. For patients with visual or cognitive impairments, adding pictures of the pills can be incredibly helpful.
- Use the "Teach-Back" Method: After explaining the medication regimen, ask the patient or their caregiver to explain it back to you in their own words (e.g., "Can you tell me which pills you need to take in the morning?"). This confirms their understanding far more effectively than a simple "Do you have any questions?".
- Schedule a Follow-Up Call: A pharmacist or nurse should call the patient within 48-72 hours post-discharge. This call is a perfect opportunity to address any new questions, confirm they have filled their prescriptions, and check for any side effects.
- Involve a Pharmacist: Studies show pharmacist-led discharge counseling significantly reduces readmissions. For instance, the Cleveland Clinic saw a 25% reduction in readmissions after implementing such a program. If possible, arrange for a pharmacist to review the final medication list with the patient before they leave.
The following infographic highlights the powerful, data-backed benefits of implementing a robust medication reconciliation and education program.
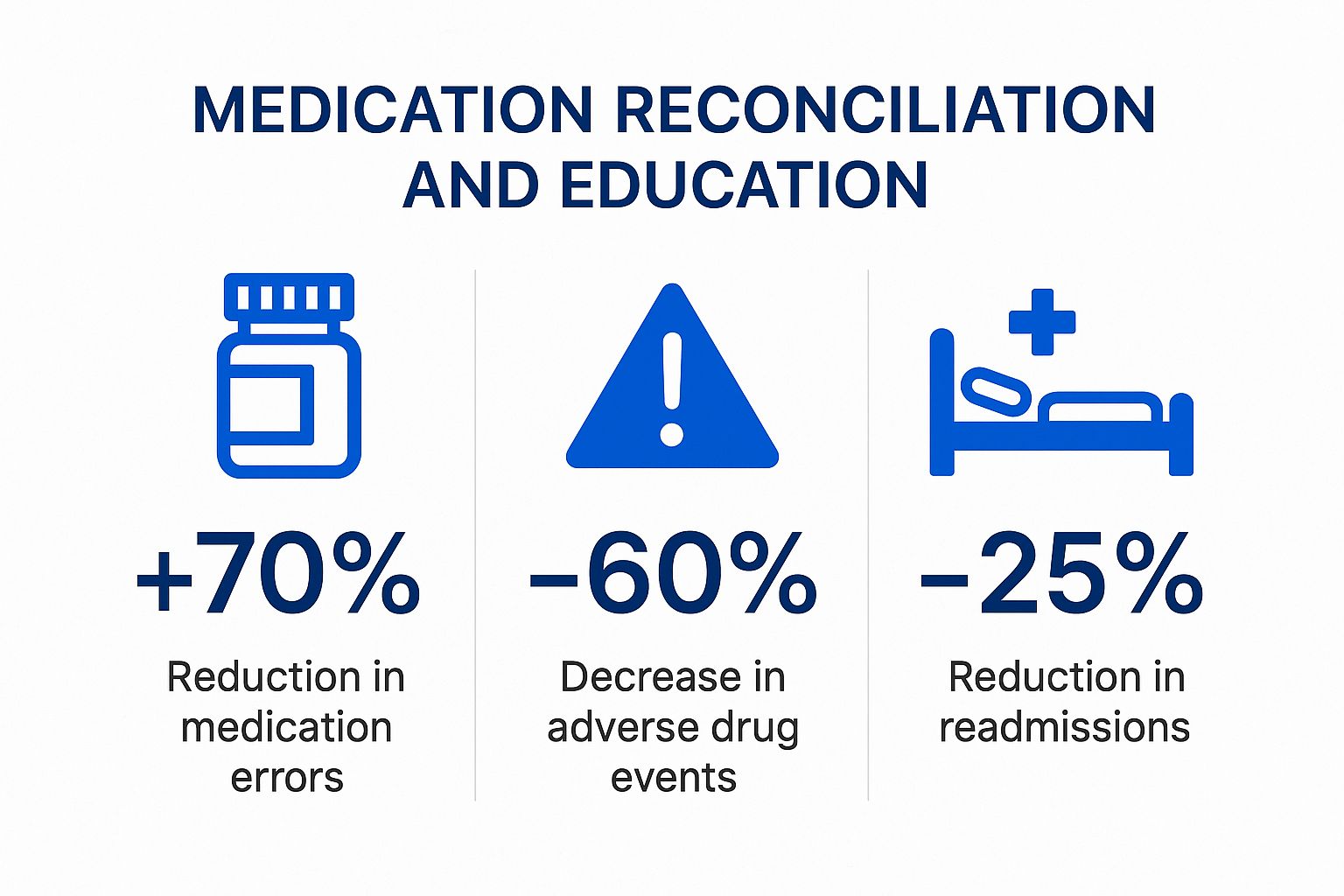
These statistics clearly demonstrate that dedicating resources to proper medication management yields significant returns in patient safety, health outcomes, and healthcare cost reduction.
2. Follow-up Care Coordination
A successful hospital discharge is not the end of the patient's care journey; it is the beginning of the next phase. Follow-up care coordination is the systematic process of arranging and managing all post-discharge medical appointments, specialist consultations, diagnostic tests, and home health services. This vital component of any discharge planning checklist ensures there are no gaps in treatment that could lead to preventable complications or hospital readmissions.

Effective coordination involves more than just handing a patient a list of phone numbers. It means proactively scheduling crucial appointments before the patient even leaves the hospital, confirming that medical records have been transmitted, and ensuring that every provider involved in the patient's ongoing care is fully informed and aligned.
Why It's a Critical Next Step
Without robust coordination, patients, especially those with complex conditions or limited health literacy, can easily fall through the cracks. Missed follow-up appointments with primary care physicians or specialists are a leading cause of adverse events and a primary driver of the "revolving door" of hospital readmissions.
Major healthcare bodies like the Centers for Medicare & Medicaid Services (CMS) and the Case Management Society of America champion structured care coordination. They recognize it as a cornerstone of value-based care, directly linking proactive follow-up to improved patient outcomes and reduced healthcare expenditures. For example, Mayo Clinic’s integrated care coordination programs have been shown to reduce readmissions by as much as 30%.
Key Insight: Think of follow-up care coordination as building a bridge from the controlled hospital environment to the patient's everyday life. Each scheduled appointment and confirmed information transfer is a plank in that bridge, ensuring a safe and stable crossing.
Practical Implementation and Actionable Tips
Translating the concept of coordination into practice requires a proactive and organized approach from the discharge team.
- Schedule Key Appointments Pre-Discharge: For high-risk patients, schedule the first primary care follow-up appointment to occur within 7 to 14 days of discharge. Do this before the patient leaves the hospital to eliminate the burden and potential for delay.
- Provide a Written Itinerary: Give the patient and their family a clear, simple document listing all scheduled appointments. This should include the date, time, provider's name, full address, and contact number.
- Ensure Information Transfer: Before any follow-up visit, confirm that the patient's discharge summary and relevant medical records have been successfully transmitted to the receiving provider. This prevents redundant testing and ensures the physician has the full clinical picture.
- Leverage Case Managers for Complex Cases: For patients with multiple comorbidities, social barriers, or complex needs, a case manager is invaluable. They can coordinate with various services, from home health aides to social workers, ensuring all aspects of the patient's well-being are addressed.
3. Patient and Caregiver Education
An effective discharge is impossible without effective education. Patient and caregiver education is a comprehensive process that empowers individuals with the knowledge and skills needed to manage their health confidently at home. This goes far beyond handing over a pamphlet; it's a structured approach to ensuring patients and their families understand the diagnosis, treatment plan, medications, and crucial warning signs to watch for.
The core objective is to bridge the information gap between the clinical setting and the patient's daily life. This part of the discharge planning checklist involves tailoring communication to the patient's health literacy, language, and cultural background, transforming complex medical information into understandable, actionable steps.
Why It's a Critical Step for Empowerment
When patients leave the hospital without a clear understanding of their condition or follow-up care, the risk of complications, anxiety, and readmission skyrockets. They may not recognize a worsening symptom or understand the importance of their medication regimen, leading to preventable health crises.
Recognized by leading bodies like the Agency for Healthcare Research and Quality (AHRQ) and the National Quality Forum, structured patient education is a cornerstone of safe care transitions. For example, Boston Medical Center’s health literacy program, "Project RED" (Re-Engineered Discharge), successfully reduced readmissions by 30% by focusing on clear, patient-centered education.
Key Insight: Patient education isn't about information delivery; it's about confirming comprehension. The goal isn't just for you to explain, but for them to understand, retain, and feel confident in their ability to manage their care.
Practical Implementation and Actionable Tips
Moving from theory to practice requires a deliberate, patient-first strategy. Integrating robust education into the discharge process is a high-impact investment in patient outcomes.
- Use the "Teach-Back" Method: This is the gold standard for confirming understanding. After explaining a concept, ask the patient or caregiver to explain it back in their own words. For instance, "We've talked about a few warning signs for infection. Can you tell me what you should be looking for?"
- Provide Multi-Format Materials: People learn differently. Supplement verbal instructions with clear, written materials, diagrams, or even short videos. Ensure materials are available in the patient's preferred language and use simple, jargon-free terms.
- Involve Family and Caregivers: The primary caregiver is an essential partner in the patient's recovery. Include them in all education sessions from the beginning, ensuring they also have a chance to ask questions and demonstrate their understanding via the teach-back method.
- Break It Down: Avoid a single, overwhelming information dump right before discharge. Conduct several short educational sessions throughout the hospital stay. This spaced learning approach improves retention and reduces patient anxiety.
The following video from the AHRQ provides an excellent overview of the teach-back method and its importance in ensuring patient understanding.
By prioritizing and structuring education, healthcare teams can transform the discharge process from a point of vulnerability into a moment of empowerment, setting patients up for a safer, healthier recovery at home.
4. Functional Assessment and Home Safety Evaluation
Returning home after a hospital stay often involves a significant change in a patient's physical or cognitive abilities. A functional assessment and home safety evaluation is a proactive process to ensure the patient can manage Activities of Daily Living (ADLs) safely within their own environment. This crucial element of a discharge planning checklist evaluates mobility, self-care skills, and fall risk, while also examining the home itself for potential hazards.
The primary goal is to bridge the gap between the patient's current capabilities and the demands of their living space. Led by occupational therapists (OTs) and physical therapists (PTs), this evaluation identifies necessary support, equipment, and modifications to prevent accidents, reduce caregiver strain, and promote a successful recovery.
Why It's a Critical Safety Step
Without a thorough assessment, patients are discharged into environments that may be unsafe or unsuitable for their new functional level. A simple staircase can become an insurmountable obstacle, a loose rug a severe fall risk, and a standard bathroom a site for a serious injury. This mismatch is a leading cause of preventable falls, emergency room visits, and hospital readmissions.
Leading organizations like the American Occupational Therapy Association (AOTA) and the CDC's Fall Prevention Program advocate for these assessments as a standard of care. For example, Mount Sinai Hospital's OT-led discharge program successfully reduced patient falls by an impressive 45% by focusing on this critical step.
Key Insight: A home safety evaluation isn't about judging a person's home; it's about adapting the environment to the person. It transforms the home from a potential obstacle course into a supportive and healing space, empowering the patient's independence.
Practical Implementation and Actionable Tips
Successfully integrating this evaluation requires a collaborative approach between the clinical team, the patient, and their family.
- Involve Therapists Early: Engage occupational and physical therapists as soon as possible after admission. They can begin assessing the patient's functional baseline and track their progress, making discharge recommendations far more accurate.
- Use a Home Safety Checklist: Provide the family with a standardized checklist to assess the home for common hazards like poor lighting, tripping hazards (cords, rugs), and lack of grab bars in the bathroom. This empowers them to make simple changes immediately.
- Provide Training on Assistive Devices: Don't just prescribe a walker or a shower chair. Ensure a therapist provides hands-on training to the patient and caregiver on how to use the equipment correctly and safely in a home-like setting before discharge.
- Connect to Community Resources: For more significant needs, like installing a ramp or a stairlift, the discharge team should connect the family with local agencies, contractors, or programs that can help with home modifications, sometimes at a reduced cost.
5. Communication with Primary Care and Specialists
A patient’s care does not end when they leave the hospital; it merely transitions. Effective communication between the hospital team and the patient’s outpatient providers is the critical handoff that ensures continuity of care. This step in a discharge planning checklist involves the systematic and timely transmission of comprehensive discharge information to the primary care physician (PCP) and any relevant specialists who will manage the patient's ongoing health.
The primary goal is to close the information gap that too often exists between inpatient and outpatient settings. This process ensures that the patient's PCP has a complete picture of the hospital stay, including final diagnoses, test results, procedural reports, medication changes, and the overall treatment plan. This prevents dangerous blind spots in the patient's continuing care.
Why It's a Critical Step in the Transition
When a PCP receives a patient back into their care without a clear and prompt discharge summary, they are essentially flying blind. They may be unaware of new medications that could interact with existing ones, or they might not know about critical test results that require immediate follow-up. This communication failure is a direct cause of medication errors, delayed treatment for unresolved issues, and preventable hospital readmissions.
Leading organizations like the Healthcare Information and Management Systems Society (HIMSS) and the Office of the National Coordinator for Health Information Technology advocate for robust interoperability standards precisely to solve this problem. Integrated systems, such as the Veterans Affairs' network, have demonstrated that seamless provider communication can reduce care gaps by over 60%.
Key Insight: Think of the discharge summary not as a final report, but as the first chapter of the patient's next phase of care. It's a bridge that connects the intensive, short-term hospital intervention with the long-term management provided by the primary care team.
Practical Implementation and Actionable Tips
Successfully bridging this communication gap requires a proactive and standardized approach. It’s about more than just sending a document; it’s about confirming receipt and ensuring clarity.
- Send Summaries Within 24-48 Hours: The “golden window” for sending a discharge summary is within 48 hours of the patient leaving the hospital. This timeliness ensures the PCP has the information before the patient's first follow-up appointment.
- Use Standardized Communication Templates: Employ a clear, standardized template (like the Transitions of Care consensus template) for all discharge summaries. This ensures key information like medication lists, pending tests, and follow-up needs are always included and easy to find.
- Include Direct Contact Information: Provide a direct phone number or secure messaging contact for the hospitalist or discharging clinician. This allows the PCP to quickly clarify any questions or concerns, avoiding delays in care.
- Confirm Receipt: Don't just send and forget. Implement a process to confirm that the receiving provider's office has received and acknowledged the discharge information. This can be an automated electronic receipt or a quick follow-up call from a case manager.
6. Social Determinants and Resource Assessment
A patient’s recovery doesn't happen in a vacuum; it happens within the context of their daily life. A comprehensive discharge planning checklist must extend beyond clinical needs to assess the social, economic, and environmental factors that profoundly impact health outcomes. This involves evaluating housing stability, food security, transportation access, and financial strain.

The core objective is to identify and mitigate non-medical barriers that could prevent a patient from following their care plan. For example, a patient cannot adhere to a heart-healthy diet if they live in a food desert, nor can they attend a follow-up appointment without reliable transportation. Addressing these social determinants is a proactive strategy to prevent complications and readmissions.
Why It's a Critical Component
Ignoring social determinants is a primary reason why well-crafted clinical plans fail. When a patient is discharged into an unstable or unsupportive environment, the risk of readmission skyrockets. A lack of food, safe housing, or social support creates stress and makes it nearly impossible to focus on recovery.
Recognizing this, organizations like the Centers for Medicare & Medicaid Services (CMS) and the National Association of Social Workers in Healthcare advocate for integrating these assessments into standard discharge protocols. Studies have shown a direct link between addressing social needs and improving health outcomes. For instance, Northwell Health reduced readmissions by 28% after implementing a social determinants screening program.
Key Insight: Treat social needs with the same urgency as clinical needs. A prescription for medication is incomplete without also addressing the patient's ability to access the pharmacy, afford the co-pay, and store the drug safely at home.
Practical Implementation and Actionable Tips
Integrating this assessment requires a systematic approach and strong community partnerships, often led by social workers or case managers.
- Use Validated Screening Tools: Implement standardized, evidence-based questionnaires to screen for risks like food insecurity, housing instability, and transportation barriers. This ensures a consistent and thorough evaluation for every patient.
- Maintain an Updated Resource Database: Develop and regularly update a localized database of community resources, including food banks, transportation services, housing assistance programs, and utility support agencies. This allows for quick and effective referrals.
- Prioritize and Address Critical Needs: It's often impossible to solve every social challenge at once. Work with the patient to identify the most critical barrier to their immediate recovery (e.g., getting transportation to their first follow-up appointment) and address that first, creating a plan to tackle other needs post-discharge.
- Partner with Social Service Agencies: Forge formal partnerships with local non-profits and social service organizations. These collaborations create a "warm handoff," ensuring the patient is successfully connected with the support they need rather than just being given a phone number.
Discharge Planning Checklist Comparison
| Item | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Medication Reconciliation and Education | High – requires dedicated staff and multi-department coordination | High – staff time, pharmacy and education materials | Significant error reduction (up to 70%), fewer readmissions, better compliance | Patients with complex medication regimens and transitions of care | Prevents adverse drug events; improves patient understanding and compliance |
| Follow-up Care Coordination | Moderate to High – coordination across multiple providers and services | Moderate – scheduling systems, case managers | Reduced 30-day readmissions (15-30%), improved patient satisfaction | High-risk patients needing timely post-discharge follow-up | Ensures continuity of care; facilitates early complication detection |
| Patient and Caregiver Education | Moderate – clinical staff time and culturally tailored materials | Moderate – educational resources, staff training | Better self-management, reduced complications, increased confidence | Patients and families requiring disease and treatment understanding | Enhances patient/caregiver confidence; reduces preventable complications |
| Functional Assessment and Home Safety Evaluation | Moderate to High – requires trained therapists and possibly home visits | Moderate – trained personnel, equipment assessments | Reduced falls and injuries, fewer emergency visits, improved independence | Patients with mobility or cognitive limitations discharged home | Prevents falls; identifies need for home modifications and equipment |
| Communication with Primary Care and Specialists | Moderate – depends on interoperable IT systems and admin coordination | Moderate – EHR systems, staff coordination | Improved info sharing (up to 80%), fewer errors, better follow-up | Patients requiring ongoing provider communication post-discharge | Prevents duplicate testing; ensures timely continuity of care plans |
| Social Determinants and Resource Assessment | High – complex coordination with community agencies | Moderate to High – social workers, resource databases | Reduced readmissions (up to 28%), improved adherence, better outcomes | Patients with social/economic barriers impacting care | Addresses root causes of disparities; connects patients to support resources |
Ensuring a Continuum of Care for Lasting Recovery
Navigating the transition from hospital to home is far more than a single event; it is the critical first step on the path to sustained healing. The comprehensive discharge planning checklist detailed throughout this article serves as a foundational roadmap, designed to empower patients, family members, and caregivers with the knowledge and tools necessary for a safe and successful recovery journey. By systematically addressing each element, you transform a potentially overwhelming process into a series of manageable, actionable steps.
Key Takeaways for a Seamless Transition
The core strength of a robust discharge plan lies in its interconnected components. No single item on the checklist stands alone; instead, each one reinforces the others to create a comprehensive safety net.
- Medication Reconciliation: Accurate medication management is non-negotiable. It prevents adverse drug events and ensures therapeutic goals are met, forming the bedrock of physical recovery.
- Coordinated Follow-up Care: Proactive scheduling of appointments with primary care physicians and specialists guarantees that the patient's progress is monitored, preventing potential complications before they become critical.
- Comprehensive Education: Empowering patients and their caregivers with clear, understandable information about the condition, warning signs, and care plan is paramount. Knowledge dispels fear and fosters confidence.
- Home Environment Safety: A functional assessment and home safety evaluation directly address the physical risks of returning home, modifying the environment to support independence and prevent falls or injuries.
- Unified Communication: Ensuring seamless information flow between the hospital team, the primary care provider, and any specialists closes dangerous communication gaps and promotes a unified approach to care.
- Holistic Support Systems: Addressing social determinants of health, from transportation needs to emotional support, acknowledges that recovery is a whole-person process, not just a medical one.
The Value of a Proactive Approach
Ultimately, mastering the elements of this discharge planning checklist is about taking control. It is a proactive strategy that significantly reduces the risk of hospital readmission, a common and often preventable setback. A well-executed plan does more than just ensure safety; it fosters a sense of security and independence for the patient while alleviating the stress and uncertainty for family caregivers. By meticulously planning for follow-up care, organizing medications, and preparing the home, you are not just checking boxes. You are building a stable bridge from the structured environment of the hospital to the comfort and familiarity of home, ensuring the continuum of care remains unbroken. This diligence is an investment in long-term health, well-being, and a higher quality of life, allowing recovery to progress smoothly and effectively long after the hospital stay has ended.
Executing a detailed discharge plan can feel overwhelming, but you don't have to do it alone. For families in New Jersey seeking professional support, NJ Caregiving offers specialized in-home services to ensure every aspect of the discharge planning checklist is managed with expertise and compassion. Visit NJ Caregiving to learn how our skilled caregivers can help create a safe, supportive, and healing environment for your loved one's return home.