When you're trying to figure out if a loved one needs more help at home, you'll often hear the terms ADLs and IADLs. They might sound like clinical jargon, but they’re actually simple, powerful tools for understanding what kind of support is truly needed.
The easiest way to think about it is this: Activities of Daily Living (ADLs) are the absolute basics of self-care, the things we must do to survive. In contrast, Instrumental Activities of Daily Living (IADLs) are the more complex tasks required to live independently in the community.
Understanding the Core Concepts of Daily Living

Getting a clear picture of these two categories is the single most important first step in assessing a loved one's ability to stay safe at home. They create a framework that helps pinpoint specific needs, which in turn guides you toward the right level of care.
What Are Activities of Daily Living (ADLs)?
ADLs are the foundational, physical skills we all need to take care of our own bodies. When someone starts struggling with these, it's a strong sign that they need direct, hands-on assistance. These are the tasks most of us do every day without even thinking about them.
For a deeper dive, you can check out our guide on the 12 activities of daily living.
The main ADLs include:
- Bathing and Hygiene: The ability to wash up, brush teeth, and manage personal cleanliness.
- Dressing: The skill of choosing appropriate clothes and putting them on.
- Eating: The physical act of getting food from the plate to one's mouth.
- Transferring: Moving from a bed to a chair, or from a wheelchair to the toilet.
- Toileting: The ability to use the restroom and manage personal continence.
What Are Instrumental Activities of Daily Living (IADLs)?
IADLs are a step up in complexity. They require more planning, organization, and critical thinking. It’s not uncommon for someone to be physically capable of all their ADLs but start having trouble with IADLs. This can often be an early sign of cognitive decline or issues with executive function.
Key IADLs cover a broader range of activities:
- Managing Finances: This includes everything from paying bills on time to creating and sticking to a budget.
- Meal Preparation: More than just eating, this involves planning meals, grocery shopping, and safely cooking.
- Medication Management: A critical task that involves taking the correct medications and dosages at the right times.
- Housekeeping: Keeping the home clean, tidy, and safe from hazards.
- Transportation: The ability to drive or independently arrange for other ways to get to appointments or run errands.
The distinction between these two categories has been a cornerstone of healthcare assessment since it was formally developed in 1969. This structure gives professionals—and families—a reliable way to measure a person's functional independence and track changes over time.
ADL vs IADL At a Glance
To make the distinction even clearer, here's a simple breakdown of the fundamental differences.
| Aspect | Activities of Daily Living (ADLs) | Instrumental Activities of Daily Living (IADLs) |
|---|---|---|
| Core Function | Basic self-care and physical survival | Living independently within a community |
| Complexity | Simple, physical tasks | Complex tasks requiring thought and planning |
| Focus | Caring for one's own body | Interacting with the home and outside world |
| Examples | Eating, dressing, bathing, toileting | Cooking, managing finances, transportation |
This table shows how ADLs are about personal, immediate needs, while IADLs involve managing a household and navigating the community. Understanding where the challenges lie helps tailor the right kind of support for your loved one.
Comparing ADLs and IADLs with Real-World Scenarios
Knowing the definitions is one thing, but seeing how these challenges play out in everyday life is what truly highlights the difference between ADL and IADL struggles. These real-world situations show families in Mercer County not just what tasks are hard, but why they’re hard—which is the key to finding the right kind of support.
The main difference often boils down to physical ability versus cognitive organization. One is about the body's capability to do something, while the other is about the mind's ability to plan and carry out a sequence of steps. This distinction is critical when you're trying to understand what a loved one truly needs.
From Eating to Meal Preparation: A Clear Contrast
The relationship between eating and cooking is a perfect example. The ability to feed oneself—the simple, physical act of getting food to your mouth and swallowing—is a core ADL. Someone might struggle with this because of tremors from Parkinson's disease or physical weakness after a stroke.
Meal preparation, on the other hand, is a much more complex IADL. It requires a whole chain of thought and action:
- Planning what to eat for the week.
- Checking the pantry to see what you already have.
- Making a shopping list and getting through the grocery store.
- Safely using a stove, oven, or microwave.
A person in the early stages of dementia may have no trouble eating but find the multi-step process of making a meal completely overwhelming.
Medication Management: A Critical IADL Scenario
Managing medications is another vital IADL that goes way beyond the simple ADL of swallowing a pill. Proper medication management involves several mentally demanding steps that are absolutely essential for a person's health and safety.
Think about what it really takes:
- Remembering to take specific medications at the right times every single day.
- Organizing pills correctly in a weekly dispenser.
- Understanding what each medication is for.
- Coordinating refills with the pharmacy before running out of a prescription.
Missing a dose or taking the wrong pill can have serious health consequences. The CDC reports that roughly 10 million adults over 65 have significant trouble with at least one daily activity, and struggles with IADLs are often the first signs to appear. For a deeper dive, our article explains what these instrumental activities of daily living fully cover.
The core difference lies in the nature of the challenge. ADL difficulties often point to a need for direct physical or hands-on support, whereas IADL struggles frequently signal underlying issues with memory, planning, and executive function.
Mobility vs. Transportation: Navigating the World
Let's look at one final comparison: the ADL of "transferring" versus the IADL of "transportation." Transferring is all about immediate, personal movement—the physical ability to get out of bed and into a chair, or to stand up from the toilet. It’s a direct measure of a person’s strength and balance within their own home.
Transportation, however, is about getting around in the wider community. This IADL involves complex tasks like:
- Safely driving a car.
- Planning a route to a doctor’s appointment.
- Figuring out public transit schedules or arranging a ride-share service.
An older adult might walk perfectly fine around their house but be unable to drive due to poor vision or cognitive changes that slow their reaction time. This contrast shows how someone can seem self-sufficient at home but still be cut off from essential community resources. Spotting these subtle differences is the first step toward building a truly comprehensive care plan.
Why IADL Challenges Are a Critical Early Warning Sign
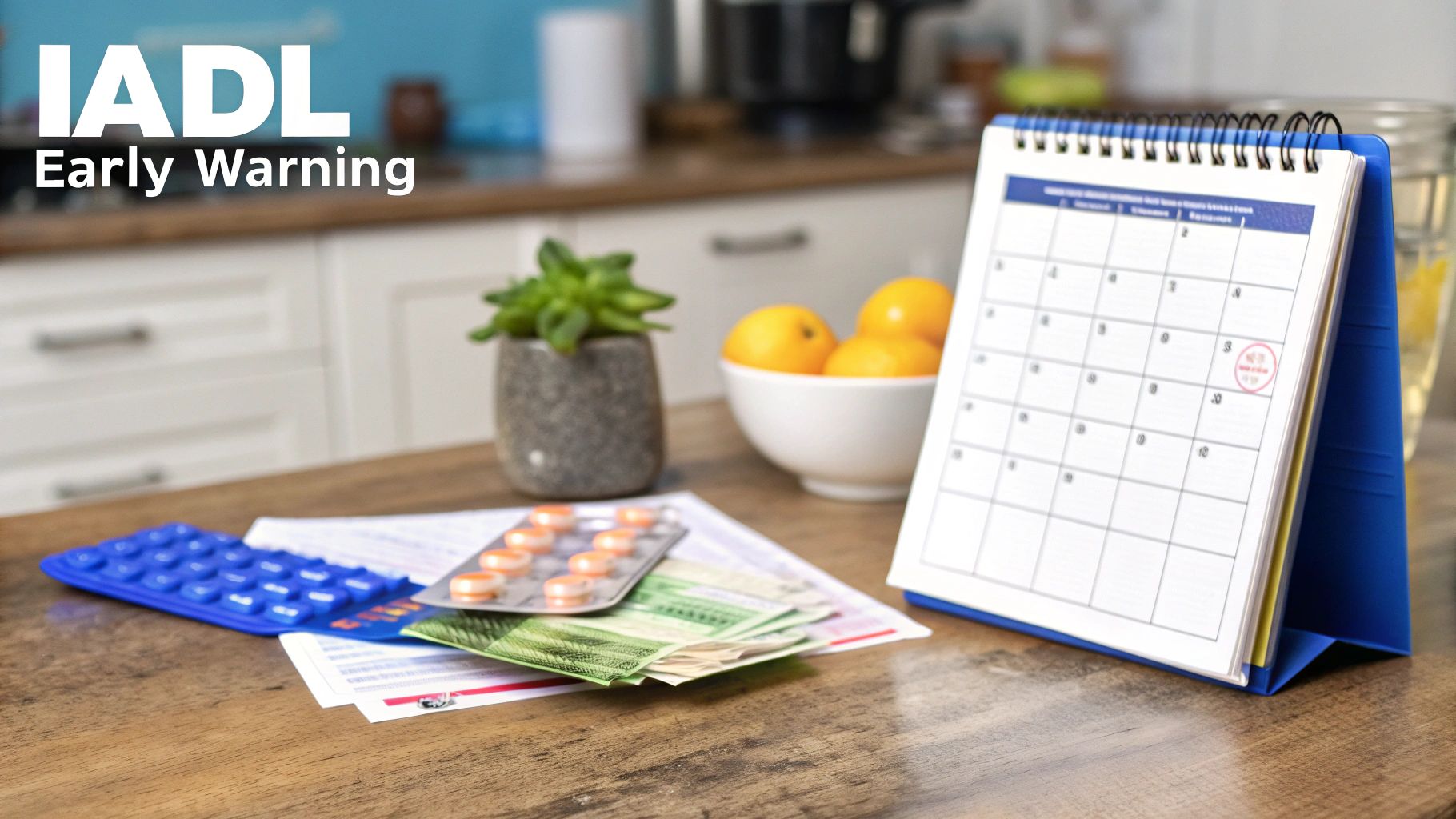
While the difference between ADL and IADL is clear, it's the order in which they decline that truly matters for families. In most situations, problems with Instrumental Activities of Daily Living (IADLs) surface long before a loved one struggles with basic self-care. This progression isn’t a coincidence—it's a critical early warning system.
When a parent starts having trouble managing their finances or getting meals on the table, it often signals a subtle shift in their cognitive or organizational skills. These small changes give families a priceless window of opportunity to step in proactively, instead of being forced to make a tough decision during a crisis like a fall or medical emergency.
Acting on these early signs isn't about taking away their independence. It’s actually about preserving it. By providing targeted support for IADL tasks, you can help a senior maintain their cherished routine, stay safer in their own home, and potentially delay or even prevent a more serious physical decline that would affect their ADLs.
The Ripple Effect of Unaddressed IADL Needs
Letting IADL challenges go unaddressed can create serious and entirely preventable risks to health and safety. A seemingly small slip-up in managing an IADL can set off a chain reaction of negative consequences that quickly puts a person’s well-being in jeopardy.
Think about the real-world impact of these struggles:
- Meal Preparation: Forgetting to buy groceries or finding cooking too overwhelming can lead straight to poor nutrition, unintended weight loss, and a weaker immune system.
- Medication Management: A single missed dose of heart medication or accidentally taking a double dose of a blood thinner can easily result in a medical emergency.
- Managing Finances: Unpaid bills can lead to utility shutoffs or even eviction, while being more vulnerable to financial scams can wipe out a lifetime of savings in an instant.
- Housekeeping: A cluttered or messy home dramatically increases the risk of falls, which remain a leading cause of serious injury for older adults.
These scenarios show exactly why IADL support is a form of preventative care. Addressing these needs early helps seniors in Princeton and the surrounding Mercer County area stay healthy, safe, and secure at home for as long as possible.
From Warning Signs to Serious Risks
The link between IADL difficulties and bigger health problems is well-documented. Population studies consistently show that IADL limitations are closely tied to chronic conditions and cognitive decline. These factors directly increase health risks, lead to more emergency room visits, and often result in unplanned moves to higher levels of care, like assisted living facilities. You can find more insights on how IADLs impact senior living options on mylifesite.net.
Viewing IADL support as a safety net is key. It's about putting measures in place that catch small problems before they grow into life-altering events, ensuring a loved one’s environment remains safe and supportive.
By recognizing and acting on these early warning signs, your family can introduce targeted in-home care that addresses the specific IADL challenges your loved one is facing. This proactive approach not only makes their home safer but also empowers them to maintain control over their lives with dignity and confidence.
How Professionals Assess ADL and IADL Capabilities
Knowing the difference between an ADL and an IADL is one thing, but how do you actually measure them? It’s not about guesswork. Healthcare professionals use specific, evidence-based tools to get an objective picture of a person's abilities. This formal assessment is the critical first step in building an effective care plan and, just as importantly, determining eligibility for services.
These evaluations aren't just a one-time snapshot. They provide a clear, numerical score that allows doctors, nurses, and care managers to track changes over time. By using the same metrics consistently, they can spot subtle declines or improvements and adjust the support plan to match. It's a data-driven approach that ensures care is both precise and responsive.
Key Assessment Tools Professionals Use
In clinical settings, two tools have become the gold standard for these evaluations: the Katz Index for ADLs and the Lawton Scale for IADLs. They’re used routinely because they provide a reliable and consistent framework for understanding a person’s functional level.
-
The Katz Index of Independence in Activities of Daily Living: This tool zeros in on the six most fundamental self-care tasks: bathing, dressing, toileting, transferring, continence, and feeding. It’s a straightforward "yes" or "no" for each one—can the person do it independently? A higher score means greater independence.
-
The Lawton Instrumental Activities of Daily Living (IADL) Scale: This scale looks at the more complex skills needed to live independently within the community. It covers eight key areas, like using a telephone, shopping, preparing meals, handling finances, and managing medications.
Healthcare providers often use both scales together to get a complete picture of a person's needs, addressing the full spectrum from basic self-care to managing a household.
A professional assessment provides an objective baseline. It transforms subjective family observations into measurable data, which is essential for developing a personalized care plan and securing insurance or Medicaid benefits.
This systematic approach helps pinpoint exactly where support is needed most. For a closer look at how these evaluations work in practice, check out our guide on the activities of daily living assessment. When families understand this process, they are much better equipped to advocate for their loved ones and ensure the care plan truly meets their needs.
How ADL and IADL Needs Impact Care Eligibility
Understanding the difference between ADL and IADL isn't just a technicality; it's what unlocks the door to getting the care you need. For families trying to figure out the financial side of senior care, an official assessment of these daily activities is what determines eligibility for long-term care insurance benefits and state-funded programs like New Jersey Medicaid.
These programs and insurance policies don't have a lot of wiggle room—their criteria are specific and non-negotiable. Most require a documented inability to perform a set number of Activities of Daily Living (ADLs) before benefits kick in. For instance, a long-term care insurance policy might require a person to be unable to perform two or three of the six core ADLs (like bathing, dressing, or getting out of a chair) without someone's help.
The Role of ADLs as Primary Qualifiers
Think of ADL limitations as the gatekeepers for most types of paid long-term care. When someone can't manage these fundamental self-care tasks, it shows a clear, undeniable need for hands-on support. From the perspective of insurance companies and government agencies, ADL dependency is the most definitive measure of whether a person can live safely on their own.
This is exactly why a formal assessment by a professional is so important. A physician or registered nurse has to document which ADLs a person can and cannot do independently. This clinical record becomes the official proof you need to file a successful claim. Without it, families often hit roadblocks, finding their applications for benefits delayed or even denied.
How IADLs Strengthen the Case for Care
While challenges with IADLs rarely trigger benefits on their own, they play a crucial supporting role. When you document struggles with tasks like managing medications, preparing meals, or handling finances, you paint a much fuller picture of a person's functional decline. It provides the critical context that strengthens the argument for needing comprehensive support.
Think of it this way: ADL needs open the door to eligibility, while IADL needs demonstrate how wide that door needs to be. Documenting IADL struggles shows that even if a person can physically eat, they cannot safely prepare a meal, which points to a serious risk of malnutrition.
This combined evidence is powerful. Documenting IADL deficits helps care planners, discharge coordinators, and insurance adjusters approve a more robust and appropriate level of in-home care services. For those looking into government funding, understanding how programs like the Assistance with Daily Life under the NDIS work can provide valuable insight into how these assessments translate into real, tangible support.
How Needs Align with Care and Funding
The level of assistance needed with ADLs and IADLs directly influences the type of care solution that's most appropriate, as well as what funding sources might be available. The table below breaks down how these needs often line up with care settings and eligibility.
| Level of Need | Common Challenges | Typical Care Solution | Likely Funding Eligibility |
|---|---|---|---|
| IADL Assistance Only | Difficulty with shopping, cooking, managing finances, or transportation. | In-home care (a few hours/week), community support programs, family assistance. | Primarily private pay; limited local grants or waivers. |
| Minor ADL Assistance | Needs help with 1-2 ADLs, like bathing or dressing, but is otherwise mostly independent. | Part-time in-home care, assisted living facility. | May qualify for some long-term care insurance benefits or Medicaid waivers. |
| Moderate ADL Assistance | Needs help with 3-4 ADLs, such as transferring, toileting, and eating. | Full-time in-home care, assisted living with higher level of care. | Likely to meet criteria for long-term care insurance and Medicaid. |
| Total ADL Dependence | Unable to perform most or all ADLs without significant hands-on support. | 24/7 in-home care, skilled nursing facility (nursing home). | Strong eligibility for all forms of long-term care funding, including Medicaid. |
Ultimately, a thorough assessment is the first step toward building a care plan that not only meets your loved one’s needs but also aligns with the benefits you’re entitled to receive.
Taking the Next Steps for In-Home Senior Care
Figuring out the subtle but critical difference between ADL and IADL needs is the first hurdle. The next, and most important, is taking action to make sure your loved one can stay safe and independent right where they want to be—at home. It all starts with paying attention and having an honest conversation.
Begin by jotting down the specific things you’ve noticed. Is your mom having a tough time with meal prep (an IADL)? Or is getting dressed in the morning becoming a real struggle (an ADL)? When you have real-world examples, it's much easier to bring up your concerns with her and her doctor. From there, a professional in-home assessment can give you an objective, clear-eyed look at her needs and create a practical roadmap for care.
Making an Informed Care Decision
The path to the right care isn't always straightforward. This decision tree helps visualize how different levels of need often point to specific solutions.
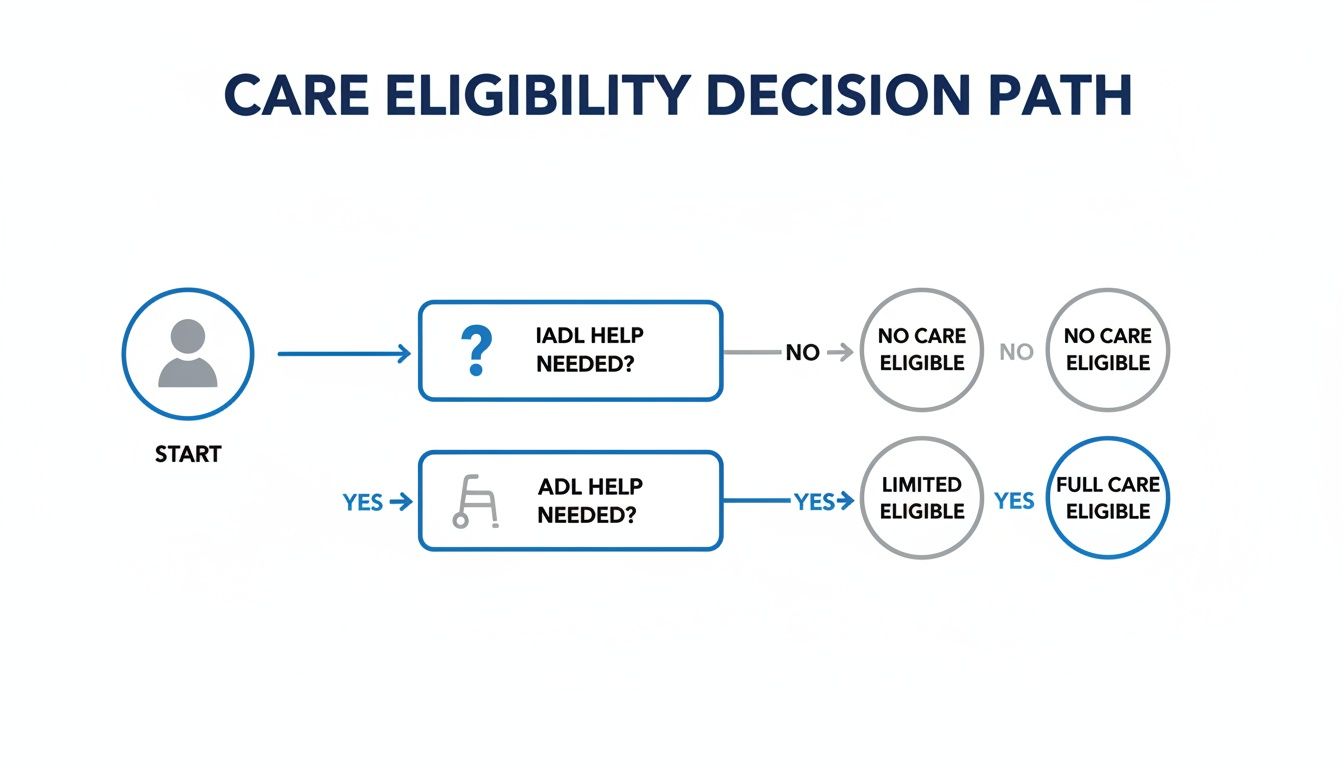
As you can see, even what seems like a minor IADL struggle is a good reason to get proactive support. Once ADL dependencies enter the picture, the need for more direct, hands-on care becomes much clearer. For anyone needing significant help with mobility and personal care, specialized equipment like hospital beds can be a game-changer for managing ADLs safely at home.
At NJ Caregiving, we build our care plans from the ground up to address both ADL and IADL requirements. It's all about boosting independence for seniors across Mercer County.
If you’ve started to notice these signs, please don’t wait for an emergency to force your hand. Reach out to our team here in Princeton, NJ, to set up a no-cost assessment. We'd be happy to talk through how we can support your family's journey.
Common Questions About ADLs and IADLs
As families start to navigate the world of senior care, it's natural to have questions. The practical differences between ADLs and IADLs can feel a bit abstract at first, but understanding them is key to getting your loved one the right support.
Here are some straightforward answers to the questions we hear most often.
Can Someone Need Help with IADLs but Not ADLs?
Yes, absolutely. This isn't just possible—it's one of the most common scenarios we see. In fact, difficulty with IADLs is often one of the first signs that a loved one needs a little more support, especially when dealing with cognitive changes or a new health issue.
Think of it this way: Your mom might still be perfectly capable of dressing and bathing herself (ADLs) but finds managing her medications or cooking a balanced meal (IADLs) overwhelming. Catching this early is a game-changer. It’s the perfect time to bring in some help, which can improve safety and keep her independent at home for much longer.
This is a critical window for proactive care. Addressing IADL challenges early can prevent crises like medication errors or poor nutrition, effectively delaying the need for more intensive, hands-on ADL support.
How Does Dementia Affect ADLs and IADLs?
Dementia typically chips away at the more complex IADLs first. This is because the disease targets executive functions—the brain's ability to plan, remember, and organize. These are the skills needed for tasks like paying bills on time, following a recipe, or remembering doctor's appointments.
Someone in the early stages of dementia might forget to pick up groceries or get confused by their budget long before they have any trouble with basic self-care. As the condition progresses, it will eventually start to impact those fundamental ADLs. The physical and cognitive ability to manage dressing, eating, or getting to the bathroom safely will decline. This predictable pattern is why it's so important to get specialized dementia care in place as soon as you notice those initial IADL struggles.
What Specific Services Support IADL Needs?
Professional in-home care is built to fill the gaps when IADLs become too challenging. The whole goal is to help seniors stay safe and independent right where they want to be—at home. These services are flexible and designed around what your loved one actually needs.
Some of the most common services that tackle IADL needs include:
- Meal Preparation: Planning and cooking healthy meals to make sure they're eating well.
- Medication Reminders: Helping them stick to their medication schedule safely.
- Transportation: Giving them a safe ride to doctor's appointments, the grocery store, or social outings.
- Grocery Shopping: Assisting with everything from making a list to putting the groceries away.
- Light Housekeeping: Keeping the home tidy and clear of clutter that could cause a fall.
These services take the stressful tasks off their plate, freeing up their energy for the people and activities they love.
If you're in Mercer County and have questions about a loved one’s changing needs, the team at NJ Caregiving is here to help. Schedule a complimentary in-home assessment today to create a personalized care plan that supports both safety and independence. Learn more at https://njcaregiving.com.