Communicating with someone who has dementia often means changing your own approach. It's less about logic and more about connection. The real pillars here are patience and simplicity, along with learning to read non-verbal cues. This isn't about correcting facts anymore; it's about validating their feelings to keep that precious bond strong.
Understanding the World of Dementia Communication

When you're trying to talk with a loved one who has dementia, conversations can quickly become frustrating and even heartbreaking. It's so important to remember that this isn't a deliberate choice on their part. I find it helpful to think of the brain as a massive, intricate switchboard. Dementia starts unplugging the wires, making it tough to process language, pull up memories, or even hold a thought.
This isn't just a personal family struggle; it's a global one. There are about 55 million people worldwide living with dementia, and that number is expected to hit 79 million by 2030. One of the most difficult parts of the disease is the breakdown in communication, which can lead to social withdrawal as memory and language skills fade. You can find more details on these statistics and what they mean for caregivers in this comprehensive report.
Once you accept this biological reality, you can start to shift from frustration to empathy. It’s the first real step.
Shifting Your Communication Mindset
The goal is no longer to have the same conversations you used to. The new focus is on connection and reassurance. It’s about meeting them in their world instead of trying to pull them back into yours.
This change in perspective is everything. When you stop taking communication breakdowns personally, you can respond with the grace and patience the situation truly calls for.
"If they say something is black and you know it's white, it's black. You go with their flow."
This idea of joining their reality is incredibly powerful. You're not "giving in"; you're choosing connection over conflict. It replaces arguments with comfort and, most importantly, preserves your loved one's dignity.
The Building Blocks of Better Conversations
Before we get into specific techniques, it’s helpful to adopt a few core principles that will guide every interaction. Think of these as the foundation—get them right, and every other strategy becomes more effective. They set the stage for more positive and less stressful communication.
The table below summarizes these core ideas. Keep these in mind, and you'll build a stronger, more compassionate communication style.
Core Principles for Dementia Communication
| Principle | Why It Matters | Simple Action |
|---|---|---|
| Empathy Over Accuracy | The emotion is more real than the fact. Correcting them causes distress and erodes trust. | If they're anxious about a non-existent appointment, say, "It sounds like you're worried. Let's sit together for a bit." |
| Patience in Pauses | Their brain needs extra time to process thoughts and find words. | Wait patiently for them to finish. Don't jump in to complete their sentences, which can make them feel inadequate. |
| Simplicity is Key | Complex sentences or multi-step requests can be overwhelming and lead to confusion. | Use short sentences and familiar words. Ask one question at a time, like "Would you like some tea?" instead of "What do you want to drink?" |
Internalizing these principles will completely change your approach. It’s less about the specific words you exchange and more about the love and respect you convey. This transforms potentially stressful interactions into moments of genuine, meaningful connection.
Creating a Calm and Supportive Environment

Before you even say a word, the room itself can set the stage for a successful conversation with a person living with dementia. Think of it this way: their brain is already working overtime to process the world. A chaotic environment can easily become a barrier, while a calm one can be a bridge to connection.
A mind affected by dementia struggles to filter out distractions. The background noise that most of us barely notice—a blaring TV, a radio playing in another room—can be incredibly confusing and overwhelming. This sensory overload can shut down a conversation before it even begins.
Setting the Stage for Success
Take a moment to scan the room before you start talking. Making a few simple adjustments can make a world of difference.
Turning off the television, moving to a quieter corner of the house, or just closing a door to a noisy hallway are powerful first steps. You're essentially creating a sanctuary of calm where their mind doesn't have to fight to focus on you. This small act is a huge sign of respect and makes a genuine connection possible.
These tweaks aren't just about being polite; they're proactive ways to lower anxiety and create a positive tone for your interaction. Here are a few impactful changes to consider:
- Cut Down on Noise: Mute the TV, turn off the radio, and close the windows to block out loud street sounds.
- Clear the Clutter: A busy, messy room can be visually overstimulating. A simpler space helps them focus on you.
- Check the Lighting: Poor lighting creates shadows that can be frightening or misread. A well-lit room is far more calming and helps them clearly see your facial expressions.
Effective communication starts with an atmosphere of safety and respect. When you control the environment, you're removing obstacles and giving the person a chance to feel secure enough to engage with you.
Your Presence and Approach
How you enter their space and your own body language are just as crucial as the physical room. Abrupt movements or approaching someone from behind can be startling, sometimes triggering a fear response.
Always try to approach from the front, where they can see you coming. This gives them a moment to process your arrival and prevents alarm. Offer gentle eye contact to show them you have their full attention.
Whenever possible, sit down so you're at their level. This is a simple, non-threatening gesture that communicates equality and warmth, making the conversation feel more like a friendly chat than an interrogation. Your calm presence is a powerful, non-verbal cue that says, "You're safe with me."
By intentionally creating a supportive space, you are already communicating care and respect. This foundation is absolutely essential for any meaningful exchange you hope to have.
7 Verbal Strategies to Foster Connection

Once the room is quiet and you have your loved one's full attention, the words you choose—and just as importantly, how you say them—can make all the difference. Think of adapting your speech as one of your most powerful tools. This isn't about winning a debate or proving a point; it’s about building a bridge.
The aim is to keep your language simple without sounding condescending. We're talking short sentences, familiar words, and a gentle, encouraging tone. It’s not "dumbing down" the conversation; it's making it accessible.
Simplify Your Questions and Instructions
Long, complicated questions can feel like an impossible puzzle for a mind already struggling to process the world. Instead of asking open-ended questions that demand a lot of memory recall, try offering simple choices.
For instance, asking, "What would you like for lunch today?" might trigger stress. They have to mentally scan all possible lunch foods and then form an opinion. A much kinder approach is to present a clear, easy choice: "Would you like soup or a sandwich?" This narrows their focus and makes the decision feel manageable.
This same idea applies to giving instructions. Rather than saying, "Let's get your coat on and then go out to sit on the porch," break it down into single steps.
- First, focus on one thing: "Let's put on your coat."
- Once that's done, move to the next step: "Now, let's go to the porch."
Embrace the Power of Patience
This is one of the hardest skills to master, but it's absolutely crucial. When you ask a question, their brain might need more time to find the right path to an answer. It’s so tempting to jump in and finish their sentence or supply the word, but this can make them feel flustered and inadequate.
Give them time. Seriously, count to ten in your head before you even think about speaking again. This patient pause is a powerful signal of respect. It shows them you value what they have to say, no matter how long it takes to come out.
The real measure of successful communication with a person living with dementia isn’t speed or perfect accuracy; it’s the emotional connection you maintain. Patience is the currency of that connection.
This mindset can transform your interactions. When you prioritize respect and understanding, you create a foundation for better care. The key is to speak slowly, use simple words, ask just one question at a time, and wait. These techniques reduce distress and dramatically improve cooperation. You can learn more about these effective interaction strategies on The Chicago School's blog.
Redirect Gently Instead of Correcting
It’s inevitable: the conversation will sometimes veer into territory that’s confusing or factually incorrect. Your first instinct will probably be to correct them. But trust me, arguing about facts with someone with dementia is rarely productive and almost always leads to frustration and agitation.
A much better strategy is to listen for the emotion behind their words and gently redirect the conversation.
- If they insist: "I need to go pick up the kids from school."
- Instead of correcting: "The kids are all grown up now, remember?"
- Try redirecting with validation: "You were such a wonderful mother. Tell me about what they were like in school."
This powerful technique is known as validation. You're acknowledging their reality and the feelings tied to it, which provides comfort and connection. You're choosing connection over correction, which is always the right call.
Speaking Volumes Without Saying a Word
When someone you love is living with dementia, the world of words can become a tangled and confusing place. As their condition progresses, you’ll find that your ability to communicate non-verbally becomes your most valuable tool.
What you say with your body, your touch, and your facial expressions will often carry much more weight and reassurance than any sentence you could put together. This is where the real connection happens—in the quiet, unspoken moments.
Even as verbal skills decline, a person's ability to read non-verbal cues often stays surprisingly sharp. A tense posture, a frustrated sigh, or a hurried pace can spark anxiety and distress, no matter how kind your words are. Your non-verbal signals truly set the emotional tone for every single interaction.
The Language of Your Body
Your very presence can speak volumes before you even say a word. A calm, open posture immediately signals that they are safe with you. A gentle smile conveys warmth and affection, cutting through any confusion.
When you simply sit beside them, you're not just sharing a space; you're offering companionship without the pressure of a conversation. It’s a powerful act.
Think about these simple, yet profound, non-verbal actions:
- Maintain gentle eye contact: This lets them know you are present and fully focused on them.
- Keep a relaxed facial expression: A soft, friendly look is a universal sign of comfort.
- Use open body language: Try to avoid crossing your arms, which can feel defensive or closed off. Instead, keep your posture relaxed and inviting.
Making these small adjustments can turn a potentially stressful moment into one of quiet connection and genuine understanding.
Holding a hand can be incredibly reassuring. Dementia can be a lonely and isolating experience, but a loving touch can connect you both on a level beyond words. Think of it as a direct line to their emotions when spoken language fails.
Using Gestures and Visual Aids
When words start to become unreliable, showing is almost always more effective than telling. Gestures and simple visual aids can bridge the communication gap, making your message clear while reducing frustration for both of you.
For instance, instead of asking, "Are you cold?" you could hold up their favorite sweater and gently rub your own arms. This visual cue, paired with a simple gesture, gives them a concrete idea to respond to, rather than a confusing abstract question.
You can use this "show, don't tell" method in so many daily situations:
- At mealtime: Instead of asking what they'd like to drink, hold up a glass of water and a carton of juice so they can point.
- Getting dressed: Lay out two shirts and point to each one, allowing them to indicate a preference with a nod or a gesture.
- Suggesting activities: Hold up a photo album or a deck of cards to offer an activity without needing any complex instructions.
By weaving these non-verbal strategies into your day, you’re speaking a language of pure emotion and intention. You are showing them they are seen, understood, and deeply cared for—which is the most important message you can ever send.
How to Handle Difficult Communication Moments
Even with the most effective communication strategies in your toolbox, there will be tough days. Moments when you feel like you're hitting a wall are a completely normal, expected part of the dementia journey. You’ll face everything from repetitive questions to conversations that seem to exist in another reality.
The secret isn’t to fight these moments. It's to learn how to move through them with grace and compassion. The most powerful tool you have is validation. This means shifting your focus from the literal meaning of their words to the emotion driving them. You aren't correcting facts; you're joining their reality to offer comfort and security.
Responding to Repetitive Questions
Hearing "What time is it?" for the tenth time in an hour can wear on anyone's patience. It's so easy to feel frustrated. But it's critical to remember that for your loved one, it often feels like the very first time they've asked. Their short-term memory simply isn't holding onto the information.
Instead of letting your frustration show ("I already told you!"), try one of these approaches:
- Answer Calmly and Simply: Each time they ask, give the same simple, reassuring answer. Your calm tone is just as important as the words.
- Write It Down: A small, erasable whiteboard or a notepad can be a game-changer. Write down the answer in large, clear letters (e.g., "Dinner is at 6:00 PM"). When they ask, you can gently smile and point to the board.
- Answer and Redirect: After you provide the answer, pivot their attention to something pleasant. "Dinner is in about an hour. While we wait, how about we look through this photo album together?"
This simple process of validating and redirecting can turn a potentially frustrating loop into a moment of connection.
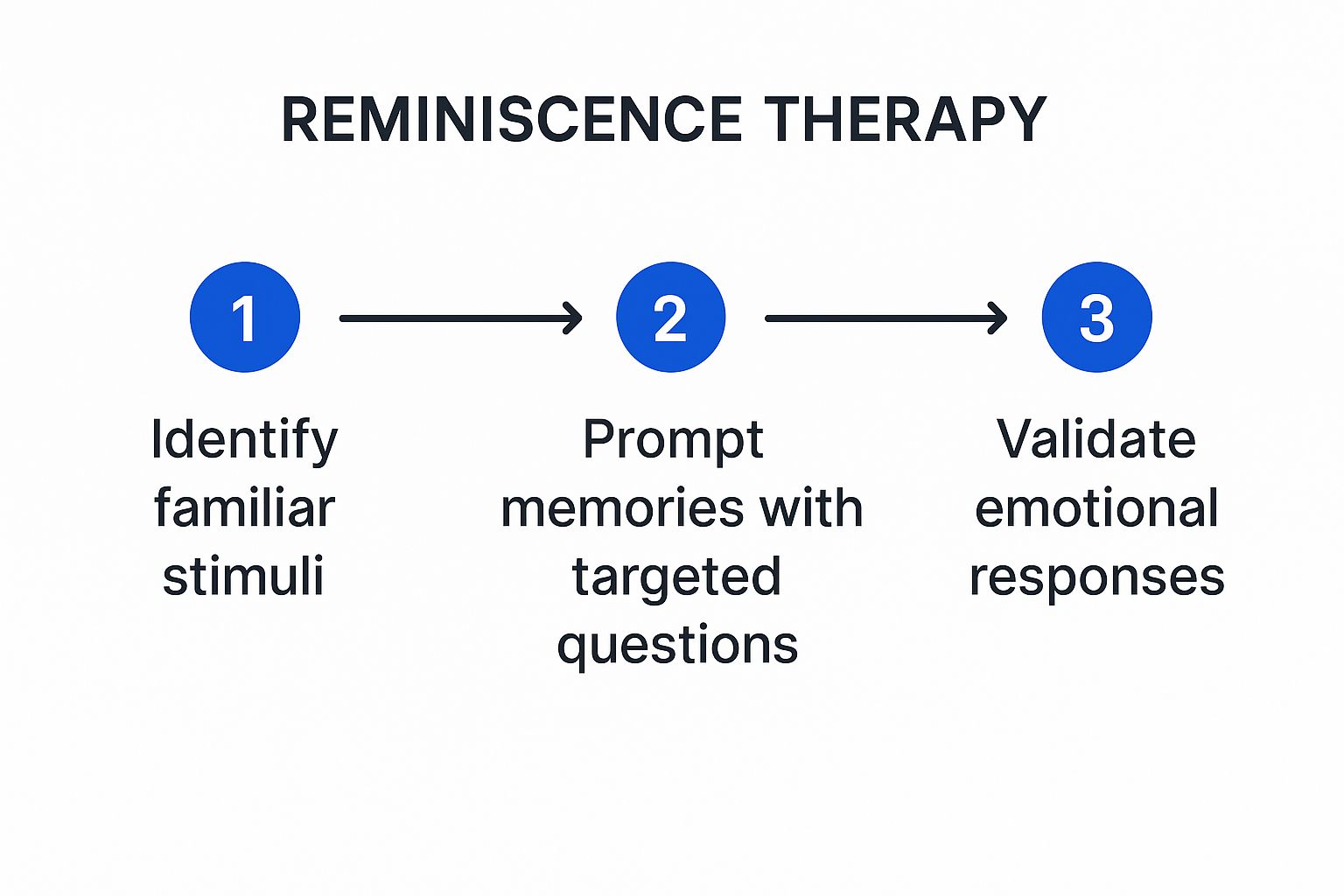
As the image shows, using familiar items and memories is a wonderful way to redirect. By validating the emotions that come up, you can transform a difficult exchange into a positive one.
Navigating Alternate Realities
This can be one of the most disorienting challenges for caregivers. Your loved one might insist they need to go home, even when they’re sitting in their own living room. Or they may talk about waiting for a visit from a parent who passed away decades ago. Arguing or correcting them is the worst thing you can do—it only leads to confusion, fear, and agitation.
A core principle of dementia care is to go with their flow. If they say the sky is green, then for that moment, it’s green. Trying to force them into your reality is a battle you cannot win and will only damage your connection.
Let's say your mother is adamant, "I need to go home right now." The emotion she's expressing is a need for security, comfort, and familiarity. Instead of arguing about where "home" is, validate that feeling.
Your Response: "Home sounds like a wonderful place. Tell me about your home. What do you love most about it?"
This simple shift in focus validates her emotional need, not the factual inaccuracy. You're connecting with her on a deeper level, de-escalating the stress and preserving her dignity.
Globally, dementia affects 6% to 10% of individuals over 65. It's vital to remember these communication struggles are caused by changes in the brain, not by choice. Adapting with patience and empathy is your best approach. For more in-depth information, you can find helpful communication strategies from the National Institutes of Health.
Your Questions on Dementia Communication Answered
As a caregiver, you're on the front lines, navigating unique and often challenging situations every single day. You have to think on your feet and respond with compassion. While we’ve covered a lot of general strategies, sometimes what you really need are straight answers to those common, painful questions that pop up.
This section is dedicated to tackling some of the toughest communication hurdles you might face. The goal is always to connect with the emotion behind their words, not just the words themselves. Offering reassurance and preserving your loved one's dignity is paramount. Remember, your calm and loving presence is the most powerful tool you have.
What Should I Do If My Loved One Doesn't Recognize Me?
This is, without a doubt, one of the most heartbreaking moments a caregiver can go through. It feels deeply personal, but it's crucial to remember that this is a symptom of the disease—it says nothing about your relationship or the love you share. The most important thing is to avoid putting them on the spot or making them feel guilty.
You'll feel a powerful urge to ask, "Don't you know who I am?" Please, resist it. This kind of question only increases their confusion and distress. Instead, meet the moment with gentle kindness and simply reintroduce yourself.
A simple, "That's okay. I'm [Your Name], and I'm someone who cares about you very much," works wonders. It's gentle, it's true, and it sidesteps any potential for conflict. Your calm presence is far more important than their ability to recall your name.
After reintroducing yourself, gently guide the interaction toward something pleasant and familiar. You could suggest looking at an old photo album, putting on a favorite song, or just sitting together quietly. The idea is to move past the difficult moment and re-establish that feeling of safety and connection.
How Do I Communicate When They Can No Longer Speak?
When words begin to fade in the later stages of dementia, communication becomes almost entirely about the senses. It's less about what you say and much more about what you do and the feeling you create. Your very presence becomes a profound form of communication.
Focus on creating a comforting sensory experience. Here are a few ways to connect without needing words:
- Comforting Touch: Gently hold their hand, stroke their arm, or brush their hair. Loving, respectful touch can be incredibly reassuring and communicates care more deeply than words ever could.
- Soothing Sounds: Keep your tone of voice warm and pleasant. The specific words you use matter far less than the comforting feeling you transmit. Play their favorite music from their younger years or read aloud from a book or poem they once loved.
- Quiet Companionship: Sometimes, the best thing you can do is just be there. Simply sitting with them in quiet companionship can ease feelings of isolation and loneliness. Your peaceful presence is a powerful comfort.
Pay close attention to their non-verbal cues. A relaxed hand, a faint smile, or leaning into your touch are all signs of comfort. Likewise, watch for any signs of distress and be ready to adjust what you're doing.
Is It Okay to Agree with Something That Isn't True?
Yes, absolutely. In the world of dementia care, this is often the kindest and most effective approach you can take. This strategy is a cornerstone of validation therapy, where you join their reality to reduce anxiety instead of trying to pull them back into ours through correction.
For example, if your loved one is anxiously waiting for their mother (who passed away years ago) to come and get them, arguing that she is gone will only bring on fresh grief and confusion. Instead, respond to the emotion they're feeling—that deep longing for their mother's comfort.
You could say something like, "Your mother is such a wonderful person. You must love her very much. Tell me about her." This validates their feelings and opens the door for a warm, reminiscent conversation, turning a moment of high anxiety into one of genuine connection. Your guiding principle should always be connection over correction.
At NJ Caregiving, we understand just how challenging these moments can be. Our team of compassionate professionals is trained to navigate these exact situations with expertise and empathy. If you need support caring for your loved one in Princeton, Hamilton, or the surrounding Mercer County area, learn more about our in-home care services.


