Being a caregiver is a powerful expression of love and commitment. But it’s also a role that carries a significant, often unseen, weight that can deeply affect your own well-being. The impact on caregiver mental health is real, stemming from the day-in, day-out emotional, physical, and psychological demands of looking after someone you care about. These challenges are a completely normal response to an extraordinary situation—not a sign that you aren't strong enough.
The Unseen Weight of Caregiving on Your Mental Health
Picture this: you start your caregiving journey with a backpack. At first, it’s light, holding just your love and dedication. But every time you make a difficult medical decision, lose a night's sleep, or feel a wave of worry, a small stone gets added. Over time, that backpack gets incredibly heavy, slowing you down and straining every part of you. This is what it feels like to manage your mental health as a caregiver.
The weight builds so gradually that many don't realize how heavy it's become until they feel completely crushed. This isn't just a feeling; it’s a reality for millions. In the United States, one in five adults is now a caregiver, a huge jump from one in seven just back in 2015. Many are also part of the "sandwich generation," trying to balance the needs of their aging loved one with their careers and raising their own families. This intense pressure has clear consequences, with studies showing it can lead to higher risks of anxiety, heart disease, and chronic stress. You can learn more about the widespread impact of caregiving on wellness in our other resources.
Your Feelings Are Valid
It’s so important to hear this: feeling overwhelmed, sad, or even resentful at times is a valid and understandable response to the pressures you're facing. These feelings don't cancel out your love or dedication.
Acknowledging the emotional toll is the first step toward protecting yourself. It’s not selfish to prioritize your own mental health; it’s absolutely essential if you want to provide sustainable, compassionate care to the person who depends on you.
Think about the safety instructions on an airplane. You’re always told to put on your own oxygen mask before helping others. If you collapse from exhaustion or emotional burnout, you can't be there for anyone else. This idea is the foundation of managing caregiver mental health.
Common Stressors and Their Impact
The specific demands of caregiving are unique and can wear down even the most resilient among us. Pinpointing how certain duties connect to mental health challenges can help you identify your own personal "stones" in that backpack. The link between your daily tasks and their psychological toll is direct and powerful.
To help you see these connections more clearly, here’s a table that breaks down some common stressors and the mental health impact they can have.
Common Stressors and Their Impact on Caregivers
| Common Caregiver Stressor | Potential Mental Health Impact |
|---|---|
| Managing Complex Medical Tasks | Constant anxiety about making a mistake or worsening a condition. |
| Witnessing a Loved One's Decline | Feelings of grief, helplessness, and anticipatory loss. |
| Financial Strain and Work Interruptions | Chronic stress over bills and long-term financial security. |
| Social Isolation and Lost Hobbies | Increased risk of depression and a diminished sense of self. |
| Navigating Family Dynamics | Frustration, resentment, and conflict with relatives who may not help. |
Looking at these connections isn't about dwelling on the negative. It's about validation. It’s proof that what you’re feeling is real, and it gives you a starting point for finding the right kind of support to lighten your load.
Recognizing the Signs of Caregiver Burnout

Caregiver burnout has a sneaky way of creeping up on you. It reminds me of that old story about the frog in a pot of water. If you drop a frog into boiling water, it jumps right out. But if you put it in cool water and slowly turn up the heat, it doesn’t sense the gradual danger until it’s too late. The decline in caregiver mental health often works just like that; the stress builds degree by degree, day by day.
There's rarely a single, dramatic moment of collapse. Instead, you might just notice you’re a little more tired than usual. A bit more irritable. Maybe you feel less connected to the life you had before. These subtle shifts are the water getting warmer. Recognizing them early is what gives you the chance to jump out of the pot before you’re completely overwhelmed.
These signs aren't just a random list of symptoms. They’re real changes in how you feel, think, and act, and they usually fall into three main buckets: emotional, physical, and behavioral.
Emotional and Mental Signs
Often, the very first signs of burnout are emotional. You might feel a constant sense of dread or anxiety when you think about your caregiving duties. It’s that feeling of being stretched so thin you think you might snap—like your emotional reserves are almost completely empty.
This kind of emotional drain can show up in a few key ways:
- Overwhelming Anxiety or Depression: This isn’t just a bad day. It’s a persistent worry, sadness, or a feeling of hopelessness that just won't lift. Some studies have even found the chronic stress levels of caregivers are comparable to those of combat veterans.
- Irritability and Anger: Do you find yourself snapping at your loved one, your family, or your friends over the smallest things? Patience is one of the first things to go when you’re emotionally exhausted.
- Loss of Motivation: The hobbies and activities you used to love might now feel like a chore. This emotional numbness can make it incredibly hard to find joy in anything.
Feeling this way is not a reflection of how much you love the person you're caring for. These are just signals that the emotional weight of your role has become too much to carry by yourself.
It's so important to remember that caregiving is a profoundly emotional job. You can feel a tangled mix of love, grief, resentment, and deep fulfillment all in the same day—sometimes all in the same hour. Giving yourself permission to feel all of it, without judgment, is a powerful act of self-compassion.
Physical Signs of Exhaustion
The mind and body are deeply connected. When your mental health is taking a hit, your physical health is almost sure to follow. Your body is keeping score of all that stress, and eventually, it starts sending up its own red flags.
Think of these physical symptoms as your body’s way of screaming for a break.
- Constant Fatigue and Sleep Problems: You might feel bone-deep tired even after what should have been a full night's sleep. Or maybe you're struggling with insomnia, waking up constantly through the night.
- Changes in Appetite or Weight: Stress can hijack your appetite. You might find yourself overeating for comfort or losing your appetite entirely, leading to major weight fluctuations.
- Weakened Immune System: Are you catching every single cold or flu that comes around? That’s no coincidence. Chronic stress tanks your immune system, making it harder for your body to fight off illness.
These aren't just small annoyances. They are signs that your body is stuck in a high-alert state, and that’s simply not sustainable in the long run.
Behavioral and Social Changes
Burnout doesn't just happen inside your head; it changes how you interact with the world and the people in it. Without even realizing it, you might start to pull away from the very support system you need most.
These shifts in your behavior are often the most obvious signs to others, even if you haven't noticed them yourself.
- Withdrawing from Friends and Social Activities: You might start turning down invitations or stop calling friends back, simply because you feel too exhausted or overwhelmed to be social.
- Neglecting Your Own Needs: This can start small, like skipping your own doctor's appointments, but it can grow into giving up on your personal goals and dreams. Your own well-being slowly slides to the bottom of the priority list.
- Feeling Resentful: It’s common to start feeling like you've sacrificed too much of your own life. This can lead to deep resentment toward the person you're caring for, or even toward other family members who you feel aren't stepping up.
If any of this sounds painfully familiar, it doesn't mean you're a bad caregiver. It means you’re human, and you're doing an incredibly demanding job that requires more support. Recognizing these signs is the first, and most important, step toward getting your own life and well-being back on track.
Understanding the High Stakes for Caregiver Well-Being

The early warning signs of burnout—that constant fatigue or flash of irritability—are just the tip of the iceberg. What lies beneath the surface is a much deeper issue, with serious consequences for both you and the person you love. Protecting your caregiver mental health isn't just about feeling a little better. It’s about recognizing the incredibly high stakes and understanding that your well-being is the very foundation of the care you provide.
Think of your personal well-being as a bank account. Every single day, you make withdrawals: emotional energy, physical strength, patience, and time. If you never make any deposits through self-care and support, that account will eventually be overdrawn. An overdrawn account can’t cover any expenses, and a burned-out caregiver simply cannot provide the effective, compassionate care their loved one deserves. The stakes are far too high to let that happen.
This isn't some isolated problem affecting only a handful of people; it's a major public health concern. The emotional and physical weight of caregiving is so significant that it can lead to serious, long-term health problems for the caregiver. When you're under constant stress, your body is stuck in a state of high alert, which takes a massive toll on your physical health over time.
The Ripple Effect on Physical and Mental Health
The prolonged stress that comes with caregiving is a direct line to significant health challenges. It's a universal issue, with caregivers everywhere facing the same struggles. What’s especially alarming is the high rate of clinical depression symptoms among caregivers.
Research reveals that a staggering 40% to 70% of caregivers show clinical symptoms of depression. That number is dramatically higher than in the general population and paints a stark picture of the mental burden involved.
This mental strain almost always spills over into physical illness. In fact, about 23% of caregivers say their duties have directly harmed their own physical health. At the same time, around 41% of caregivers report low overall well-being, a figure 32% higher than those who aren't in a caregiving role. These aren't just statistics; they represent millions of dedicated people whose health is genuinely at risk. You can dig into more caregiver trends and statistics to see just how widespread this issue is.
This link between mental and physical health can create a dangerous cycle. As your mental health slips, you have less energy to look after your physical needs, which in turn makes your mental state even worse.
More Than Just Time: The Broader Sacrifices
Beyond the immediate health impacts, the sacrifices of caregiving often creep into every corner of your life, creating a cascade of other stressors. These losses are just as real and can feed directly into feelings of burnout and resentment.
These broader sacrifices often include:
- Financial Strain: Many caregivers have to cut back their work hours, pass on promotions, or even leave their jobs entirely. This loss of income, paired with the extra costs of care, can create immense financial pressure and anxiety about the future.
- Social Isolation: The constant demands of caregiving leave very little time for friends, hobbies, or just getting out of the house. Over time, this can lead to profound loneliness and the feeling that you’ve lost your own identity outside of being "the caregiver."
- Strained Family Relationships: When one person shoulders most of the caregiving duties, it can cause friction and resentment with siblings or other relatives who may not fully grasp the day-to-day burden.
These compounding challenges make it clear why self-care isn't a luxury—it is a non-negotiable requirement of the job. It’s the act of making those crucial deposits back into your own well-being account so you can continue providing the loving support your family member needs. Understanding these high stakes is the first step toward giving yourself permission to prioritize your own health, guilt-free.
Practical Self-Care Strategies That Actually Work
Knowing you need to practice self-care is one thing. Finding the time and energy to actually do it is a whole different ballgame. For caregivers, generic advice like “take a vacation” can feel completely out of touch.
Real self-care isn't about grand gestures. It's about weaving small, sustainable moments of relief into an already packed schedule. Improving your caregiver mental health starts with practical, bite-sized actions that are realistic for your life right now. Think of it as building a toolkit of strategies you can grab on the toughest days to recharge your batteries, even if it’s just for five minutes.
The Five-Minute Reset
When overwhelm hits, you don’t need an hour of silent meditation to get back on track. The “five-minute reset” is a surprisingly powerful way to calm your nervous system right in the middle of a chaotic day. It’s a conscious pause designed to break the stress cycle before it spirals.
Here’s all you have to do:
- Find a quiet space. This doesn't have to be a zen garden—your car, the bathroom, or even just stepping into another room works perfectly.
- Set a timer for five minutes. Using your phone means you won't be tempted to watch the clock.
- Focus on your breath. Close your eyes if you're comfortable. Take a slow, deep breath in through your nose (count to four), hold it gently (count to four), and then exhale slowly through your mouth (count to six).
- Keep this breathing pattern going for the full five minutes. If your mind wanders (and it will!), just gently guide it back to your breath without judgment.
This simple act can physically lower your heart rate and stress hormones, giving your brain a crucial break from the high-alert state that defines so much of caregiving.
Build Your Support Roster
Let’s be clear: you cannot and should not do this alone. So many caregivers feel guilty asking for help, but building a "support roster" is actually a sign of incredible strength and smart planning. This isn’t just about formal respite care; it's about creating a network of people who can chip in with small, specific tasks to lighten your load.
Think of it like coaching a team where every player has a small, manageable role.
- The Errand Runner: A neighbor or friend who can grab a prescription or a few groceries for you once a week.
- The Companion Sitter: A family member who can sit with your loved one for just one hour so you can take a walk, go to an appointment, or just sit in silence.
- The Emotional Check-In: A friend you can call who just listens without trying to "fix" anything.
- The Meal Provider: A relative who can drop off a casserole or some soup every now and then.
By asking for small, defined favors, you make it much easier for people to say yes. This distributes the weight of responsibility, preventing any one person—especially you—from burning out.
The goal of self-care is not to get to a place where you no longer need help. The goal is to build a life where asking for and receiving help becomes a normal, guilt-free part of your routine.
Master the Art of Setting Boundaries
Boundaries are the invisible guardrails that protect your caregiver mental health. They are the rules you set for yourself and with others to shield your energy, time, and emotional well-being. Without them, it’s all too easy to give until you have absolutely nothing left.
Setting boundaries can feel awkward, especially with family, but it’s a critical skill for survival.
- Learn to say "no." You are not obligated to agree to every request. A polite, "I'm sorry, I can't manage that right now" is a complete sentence. No further explanation is needed.
- Set visiting hours. If people want to visit, give them a specific window of time that works for you and your loved one. This stops unexpected drop-ins from derailing your entire day.
- Delegate specific responsibilities. Instead of a vague "I need more help," approach family members with concrete tasks. Try saying, "Could you take charge of paying the bills this month?" or "Can you be responsible for all the yard work?"
Protecting your time and energy isn't selfish—it's strategic. These small, practical steps, when you practice them consistently, can make a monumental difference. They help you hold onto the very compassion that led you to become a caregiver in the first place.
Building Your Support System and Finding Help
Self-care is your first line of defense, but let’s be honest: improving caregiver mental health isn't a journey you can or should take alone. One of the most damaging myths out there is that asking for help means you’ve failed. It’s exactly the opposite. Reaching out is a sign of incredible strength and smart planning—it's you recognizing the sheer scale of your role and acknowledging that you’re human, with real limits.
Think of building a support system like building a bridge. A single beam will buckle under pressure. But a whole network of interconnected supports? That can handle just about anything. When you accept help, you're just distributing the load so that one single point—you—doesn't collapse. Making that mental shift is the key to moving from just surviving to actually thriving.
The great news is that support comes in all shapes and sizes. It's not about finding one perfect solution. It's about weaving together a patchwork of help from different people and places to create a safety net. That way, if one support isn’t available, others are right there to catch you.
Informal Support: Your Inner Circle
Your first and most immediate support often comes from your informal network—your family and friends. These are the people who already love you. The thing is, they often don’t know how to help, or they might worry about overstepping. The secret is to be direct and specific.
Instead of a vague, "I'm just so overwhelmed," try making a concrete request they can easily say "yes" to:
- "Could you possibly sit with Mom for an hour on Tuesday afternoon? I'd love to go to the grocery store by myself for once."
- "Would you be able to drop off a meal for us one night next week? It would be a massive help."
- "Can I call you on Friday just to vent for 15 minutes? I don’t need you to fix anything, just listen."
Small, manageable asks like these make it easy for people to pitch in. They feel helpful, and you get a real, tangible break. This isn't about being a burden; it's about inviting them to be part of the care team in a way that works for everyone.
Formal Support: Professional Guidance
While your inner circle is essential, sometimes you need support from people with specialized training. Formal support systems are built to tackle the specific challenges of caregiving, offering tools and perspectives your friends and family simply can't.
And you are far from alone in needing it. Caregiving is a global reality, with an estimated 260 million people worldwide looking after family members. This role frequently leads to intense psychological stress, anxiety, and major financial hits from missed work or having to retire early. The global impact of caregiving is staggering, and it's worth understanding the full scope of these challenges.
Connecting with others who truly "get it" can be one of the most powerful balms for a stressed caregiver. You realize you are not alone in your feelings of frustration, grief, or exhaustion, which can instantly lift a tremendous weight.
This is exactly where professional resources come in:
- Support Groups: These are safe spaces to share what you're going through with other caregivers. That peer connection is a powerful antidote to the profound isolation so many feel.
- Therapy or Counseling: A mental health professional can give you personalized strategies for managing stress, working through tough emotions like grief and guilt, and navigating complicated family dynamics.
- Respite Care Services: This is a non-negotiable. Professional services, like those from NJ Caregiving, give you a necessary break, knowing your loved one is in capable hands. This isn’t a luxury; it's a critical part of making caregiving sustainable.
Just look at how much support groups can impact stress levels, depending on how often caregivers attend.
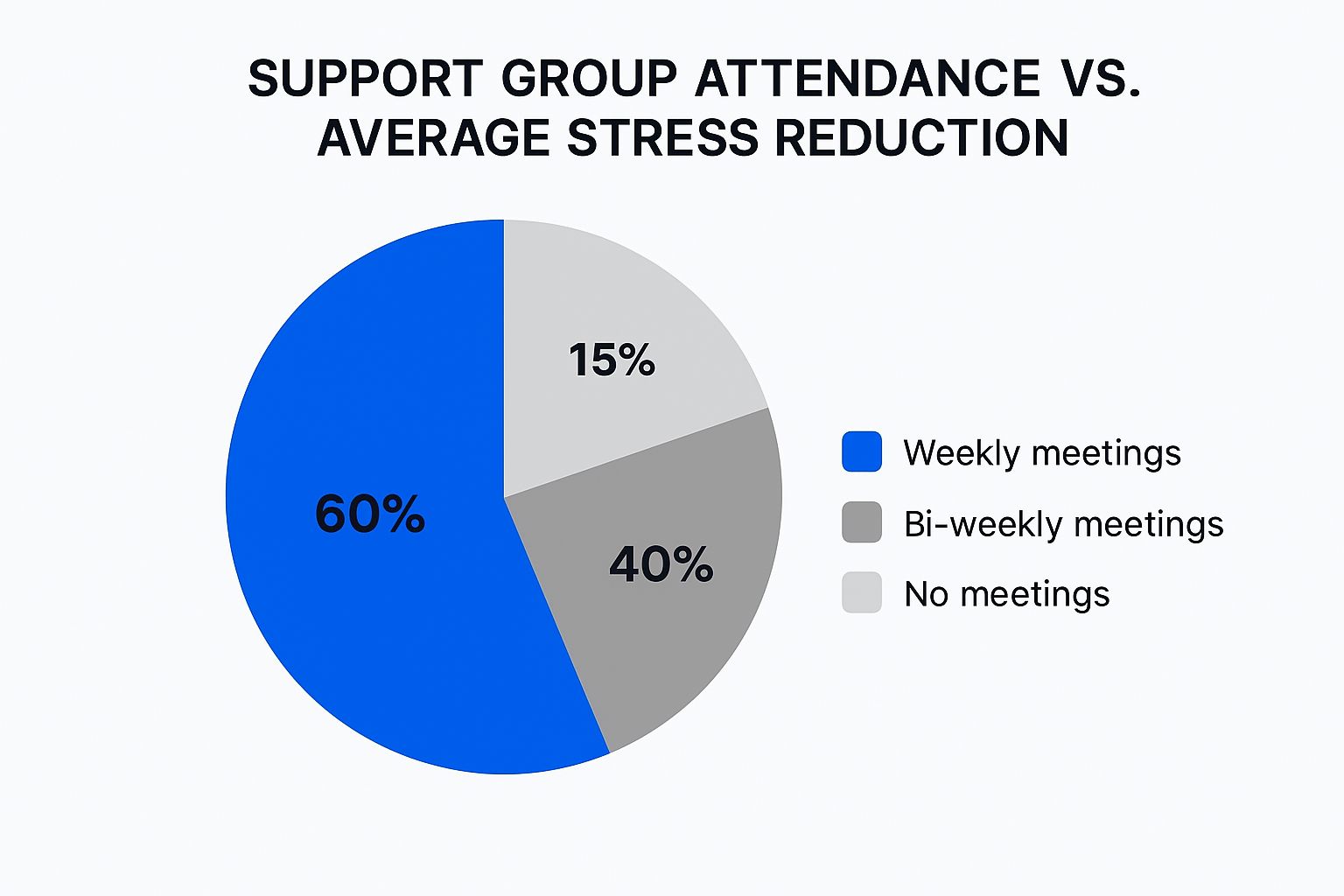
The data tells a clear story: the more you engage with a support system, the more your stress levels drop. It's a direct and powerful connection.
Tapping Into Community Resources
Beyond your friends and formal services lies a whole world of community-based support. Many local non-profits, faith-based organizations, and community centers have programs designed specifically for caregivers and older adults. These can include anything from free educational workshops and transportation services to "friendly visitor" programs.
A great starting point is your local Area Agency on Aging or a quick online search for caregiver resources in your town. You might be shocked at how many programs are available, often at little to no cost.
To help you navigate these options, here’s a quick guide to the different kinds of support and where you might find them.
Types of Caregiver Support and Where to Find Them
| Type of Support | What It Looks Like | How to Access It |
|---|---|---|
| Informal Support | Help from friends, family, and neighbors with tasks like errands, meal prep, or just providing a listening ear. | Be direct and specific with your requests. Use tools like shared calendars or group chats to coordinate. |
| Peer Support | Connecting with other caregivers who understand your daily reality. Offered through in-person or online groups. | Search online for "caregiver support groups near me." Ask your doctor or local hospital for recommendations. |
| Professional Counseling | One-on-one therapy to develop coping strategies, manage stress, and process complex emotions. | Ask your primary care doctor for a referral. Check with your insurance provider for covered mental health professionals. |
| Respite Care | Short-term relief provided by professional in-home aides or at adult day centers, giving you a break. | Contact local home care agencies like NJ Caregiving. Your Area Agency on Aging can provide a list of local providers. |
| Community Services | Local programs offering practical help like transportation, meal delivery (e.g., Meals on Wheels), or legal aid. | Contact your local Area Agency on Aging or dial 2-1-1 to connect with local services. |
Building your support system is an ongoing process of discovery. By combining informal, formal, and community support, you create a robust network that protects your caregiver mental health and ultimately enables you to provide the best possible care for your loved one.
Of all the challenges that come with being a caregiver, the questions that keep you up at night are often the hardest. Beyond the endless to-do lists, you're likely wrestling with heavy emotions and tough situations that feel difficult, or even impossible, to talk about.
This section tackles some of those common questions head-on. If you've been struggling with these thoughts, please know you are absolutely not alone. Getting straight answers is a vital first step toward managing the emotional weight of your role.

How Do I Deal With Overwhelming Guilt?
Guilt is a constant, unwelcome companion for so many caregivers. It can show up as feeling resentful, losing your patience, or just wishing for a day off. It's a corrosive feeling that can eat away at your confidence.
The first step is to recognize that this guilt often comes from holding yourself to an impossible standard. You are a human being with real limits, not a superhero. Giving yourself permission to have complex, messy emotions is key to letting that guilt go.
Remember this: Feeling frustrated, angry, or nostalgic for your old life does not cancel out your love or dedication. It's a completely normal human response to a profoundly demanding situation. It doesn’t make you a bad caregiver—it just makes you a person.
Try to pinpoint the specific thought fueling the guilt. Is it something like, "I should be able to do all of this by myself without feeling stressed"? Take a moment and challenge that idea. Would you ever expect a friend in your exact shoes to handle everything alone, 24/7, with a smile? Offer yourself that same kindness.
What If My Family Doesn’t Help Or Understand?
Few things sting more than feeling like your own family has left you to handle the burden alone. It's incredibly disheartening when siblings or relatives just don't seem to get it or offer any real help.
You can spend a lifetime of energy trying to make them "understand," but it's often a losing battle. A better approach is to shift your focus from changing their minds to setting firm boundaries and making direct, specific requests.
Here's how that might look:
- Stop Explaining, Start Asking: Instead of pouring your heart out in long, emotional texts, make concrete asks. "Can you be in charge of all prescription refills this month?" is far more effective than, "You have no idea how hard this is for me."
- Give Them a Job: If a relative offers a vague, "Let me know if you need anything," give them a specific task. "It would be a massive help if you could handle the grocery shopping every Tuesday."
- Accept Their Limits: This is the hard part. You can't force someone to step up. If they consistently say no, it's painful, but accepting it frees you from wasting emotional energy. You can then focus on building a support system with people who do show up.
This strategy protects your own caregiver mental health by centering on what you can actually control—your actions and requests, not their reactions.
How Can I Find Affordable Mental Health Support?
Looking after your own mental health is non-negotiable, but the potential cost can feel like just another hurdle. Fortunately, affordable and even free support is out there if you know where to look.
First, call your health insurance provider. You might be surprised. Many plans now offer much better coverage for therapy, including telehealth sessions with low co-pays. It's always worth checking before assuming it's too expensive.
Also, be sure to explore these low-cost options:
- Community Health Centers: These federally funded centers often provide mental health services on a sliding scale based on your income.
- University Training Clinics: Local universities with psychology or social work programs often have clinics. You can receive excellent counseling from graduate students (supervised by licensed pros) for a very low fee.
- Non-Profit Organizations: Groups like the National Alliance on Mental Illness (NAMI) provide free support groups and classes. While it's not therapy, connecting with peers is incredibly powerful.
- Online Therapy Platforms: Many online services have subscription models that can be more budget-friendly than traditional in-person therapy, with the huge bonus of being accessible from home.
Don't ever underestimate the power of simply talking to someone who gets it. Finding a local or online caregiver support group can be a game-changer. Being heard and validated by others on the same journey can be profoundly healing.
Navigating these challenges is a heavy burden to carry alone. NJ Caregiving is here to help lift some of that weight. Our professional respite care services give you the essential breaks you need to rest, recharge, and focus on your own well-being, knowing your loved one is in compassionate, expert hands. Learn more about how we can support your family at https://njcaregiving.com.


