When you decide that home care for seniors with dementia is the right path, you’re choosing to keep them in a familiar, comforting space. This simple decision can make a world of difference, dramatically reducing the agitation and confusion that often come with the condition. It’s about prioritizing their dignity and sense of self by holding onto the routines and connections that anchor them.
Why Home Care Is a Lifeline for Dementia Patients

When a loved one is diagnosed with dementia, families are suddenly faced with incredibly tough decisions about their care. While moving to a residential facility is one option, more and more families are recognizing the profound benefits of aging in place.
Think about it: the familiar sights, sounds, and rhythms of home provide a powerful anchor in a world that can feel increasingly disorienting. This stability isn't just a "nice-to-have"—it's a critical part of managing dementia effectively. Dropping someone into an unfamiliar environment can ramp up anxiety and trigger difficult behaviors. A home filled with cherished memories, on the other hand, helps preserve their identity and connection to their own life story.
The Power of Familiarity and One-on-One Support
For someone living with dementia, the simple act of waking up in their own bed or sipping coffee from their favorite mug offers a deep sense of security. This consistency minimizes stress and can even support cognitive function by freeing up the mental energy they’d otherwise spend trying to navigate a new place.
Beyond the physical environment, professional in-home care provides something that larger facilities often can't: dedicated, one-on-one attention. A consistent caregiver, like the ones we have at NJ Caregiving, builds a real, trusting relationship with your loved one. This unique bond allows the caregiver to:
- Spot subtle shifts in mood or health that might otherwise be missed.
- Adapt activities and conversations to how your loved one is feeling that specific day.
- Offer genuine companionship that helps fight the loneliness and isolation so common with dementia.
The advantages of this approach are clear for both the senior and their family. This table breaks down some of the most significant benefits.
Key Benefits of In-Home Dementia Care
| Benefit | Impact on Senior with Dementia | Benefit for Family Caregivers |
|---|---|---|
| Familiar Environment | Reduces confusion, anxiety, and agitation. Helps maintain a sense of identity and security. | Peace of mind knowing their loved one is in a comfortable, stress-reducing setting. |
| Personalized, One-on-One Care | Care is tailored to their specific needs, preferences, and daily rhythms. Fosters a strong, trusting bond. | Confidence that care is consistent and attentive, not spread thin among many residents. |
| Maintained Independence | Allows for greater autonomy in daily activities and routines, preserving dignity. | Less guilt and stress associated with uprooting a loved one from their home. |
| Slower Cognitive Decline | The familiar and engaging environment can help slow the progression of cognitive symptoms. | Reduced worry about the rapid decline that can occur in unfamiliar or chaotic settings. |
| Family Involvement | Easier for family to visit, participate in care, and stay connected without strict visiting hours. | Greater flexibility and ability to remain an active part of the loved one’s daily life. |
Ultimately, choosing home care helps maintain a sense of normalcy and connection that is invaluable.
A Growing Trend Supported by Data
The preference for keeping loved ones at home isn't just anecdotal. Data shows that the use of home health care by people with dementia shot up between 2010 and 2019. In fact, individuals with dementia are twice as likely to need these services, and they make up about 30% of all home health care users. That's a huge number, and it shows just how vital this type of support is. You can dig into more of these findings on home care trends for dementia.
For many families, home care isn't just a service; it's a strategy. It's about creating a sustainable support system that honors the individual's past, supports their present needs, and provides peace of mind for the future.
This approach completely reframes the care experience. Instead of focusing only on what's been lost, it emphasizes preserving quality of life and creating moments of genuine connection. With the right support, home truly can be the safest and most therapeutic place for a senior with dementia.
Creating a Safe and Calming Home Environment

When you're providing home care for seniors with dementia, one of the most immediate and impactful things you can do is transform their living space into a safe haven. A home that feels secure and predictable can dramatically reduce anxiety and agitation, which goes a long way toward promoting independence.
This isn't about making the home feel like a sterile, clinical setting. Far from it. It’s about making thoughtful, often subtle, adjustments that address the real-world challenges of cognitive decline. Every change, from minimizing fall risks to creating a more sensory-friendly atmosphere, helps improve their quality of life.
Starting with the Biggest Risks
Fall prevention is job number one. For a person with dementia, changes in visual perception and balance can turn everyday objects into serious hazards. The best way to start is by walking through the home with a critical eye, specifically looking for anything that could cause a trip or a slip.
Think about the most-traveled paths in the house—from the bedroom to the bathroom, or the living room to the kitchen. These areas need to be completely clear.
- Clear out clutter and trip hazards. This means getting rid of loose rugs, moving unnecessary furniture out of walkways, and securing any electrical cords.
- Boost the lighting. Dementia can affect eyesight and depth perception. Adding nightlights in hallways and bathrooms makes a huge difference. You also want to ensure every room is brightly and evenly lit to get rid of confusing shadows.
- Secure the floors. Tack down the edges of carpets and use non-slip mats in the kitchen and bathroom. It's also wise to avoid high-gloss waxes on floors that can create a distracting and disorienting glare.
Getting these fundamentals right creates a baseline of safety you can build on room by room.
A well-adapted home does more than just prevent accidents; it actively communicates safety and comfort to a person with dementia. By reducing environmental stressors, you create more space for calm, connection, and positive interaction.
A Room-by-Room Approach to Dementia Proofing
Once you've handled the most obvious hazards, you can zoom in on specific rooms where risks tend to be concentrated. For a deeper dive, consulting a comprehensive home safety guide can give you even more detailed strategies.
The Kitchen
A kitchen is full of potential dangers, from sharp objects to hot appliances. The goal is to allow safe use while securing anything that could cause harm.
- Install safety knobs on the stove or look into an automatic shut-off device.
- Store sharp utensils, knives, and small appliances in locked drawers or out-of-reach cabinets.
- Get rid of any artificial food items, like wax fruit, that could easily be mistaken for the real thing.
- Label cabinets with simple pictures or words (e.g., "Plates," "Cups") to make finding things easier.
The Bathroom
With its wet surfaces, the bathroom is a high-risk area for falls. It can also be a source of confusion.
- Install Grab Bars: Make sure they are securely mounted next to the toilet and both inside and outside the shower or tub.
- Use a Shower Chair and Handheld Showerhead: This combination makes bathing much safer and less physically taxing for everyone involved.
- Set the Water Heater to a Safe Temperature: Adjusting it to 120°F (49°C) or lower is a simple way to prevent accidental burns.
- Simplify the Space: Clear away all the extra bottles and products. Keep only the daily essentials out where they are easy to see and access.
Creating a Calming and Navigable Space
Safety is also about reducing confusion and emotional distress. Simple visual cues can make a home much easier for someone with dementia to navigate on their own.
For example, using color to create contrast can be incredibly helpful. A brightly colored toilet seat stands out against a white floor and toilet. A dark-colored placemat on a light-colored table helps define where to eat.
Finally, think about managing sensory input. A blaring TV or constant background noise can be overstimulating and trigger agitation. Try to create a calm auditory environment, maybe with soft, familiar music instead. It can also help to minimize mirrors, as a person with dementia might find their own reflection confusing or even frightening. Each of these small changes adds up, creating a profoundly more supportive and secure home for your loved one.
Establishing Comforting Daily Routines and Activities
For someone living with dementia, the world can start to feel unpredictable, even a little chaotic. That’s why a consistent daily routine isn't just about scheduling—it's a lifeline. It creates a sense of security and calm that can make all the difference, reducing anxiety and minimizing some of the more challenging behaviors we often see.
But let's be clear: this isn't about a rigid, minute-by-minute itinerary. The goal is to create a gentle, flexible structure that flows with the good days and the not-so-good days. A successful routine in home care for seniors with dementia is built around your loved one's lifelong habits and preferences, adapting as their abilities change. Think rhythm, not a rulebook.
The Foundation of a Gentle Routine
The best place to start is with the basics that have always given shape to a person's day: waking up, mealtimes, and bedtime. These are familiar, grounding anchors. Keeping these moments at roughly the same time each day helps regulate their internal clock and brings a sense of normalcy.
Think back to what your loved one’s life was like before the diagnosis. Was your dad an early riser who never missed the morning paper with his coffee? Did your mom prefer a slow, quiet start to her day? Weaving these old, comforting habits into the present makes the day feel natural, not like a list of chores.
- Morning: Ease into the day. Rushing creates stress. Allow plenty of time for waking up naturally, using the bathroom, and getting dressed without pressure.
- Afternoon: This is often a great window for more engaging activities. A short walk outside, listening to a favorite album, or working on a simple puzzle can provide just the right amount of stimulation.
- Evening: The focus here is on winding down. Dim the lights, put on some soft, familiar music, and steer clear of loud or confusing TV shows that might be agitating before bed.
This simple framework gives the day a predictable shape while leaving plenty of room to adjust based on how they're feeling.
Navigating Activities of Daily Living with Dignity
Let's be honest—the basic "Activities of Daily Living" (ADLs) like bathing, dressing, and eating can become major flashpoints. It's easy for these moments to turn into a struggle. The key is to shift your approach and turn these necessary tasks into moments of connection, always preserving your loved one’s dignity.
How you communicate and prepare can change everything. Instead of announcing, "It's time for your shower," which can feel jarring and demanding, try a softer invitation. Something like, "Let's go get you warmed up and refreshed," as you gently guide them toward a bathroom you've already prepped and warmed, feels much more collaborative.
When helping with personal care, try to see yourself as a supportive partner, not a director. Break every task into small, simple steps, keep your voice calm, and offer choices whenever you can. It gives them back a sense of control.
For instance, when it's time to get dressed, don't just pick an outfit. Lay out two shirts and ask, "Would you like to wear the blue one or the red one today?" This simple choice reinforces their autonomy and can head off a potential power struggle before it even starts.
Fostering Purpose with Meaningful Activities
Boredom is the enemy. A lack of stimulation is often the real culprit behind restlessness and agitation. The right activities don't just pass the time; they provide a genuine sense of purpose and joy.
The trick is to match the activity to their current abilities and past interests. If something is too hard, it will only lead to frustration. If it's too simple, it can feel demeaning. Always focus on the process and the enjoyment of the moment, not the final result.
Ideas for Simple, Engaging Activities
- Sorting and Organizing: Many people with dementia find repetitive, tactile tasks incredibly soothing. Give them a basket of colorful socks to fold and sort, a bowl of mixed nuts to separate, or a stack of junk mail to organize.
- Music and Memory: Never underestimate the power of music. Create a playlist of songs from their teenage years or early 20s. Music can tap into deep-seated memories and emotions in a way nothing else can, instantly calming agitation and creating beautiful moments of connection.
- Simple Household Chores: Asking for help with familiar tasks like wiping the table, folding towels, or watering plants can make someone feel useful and included in the life of the home.
- Sensory Stimulation: Sometimes, the simplest things work best. A soft blanket, a smooth stone to hold, or the scent of a familiar hand lotion can be incredibly calming and grounding.
For more structured ideas, our team has put together a great resource. You can learn more about free printable activities for dementia patients in our guide to find things that might resonate with your loved one. The real goal is to create small moments of success and enjoyment. In dementia care, those moments are everything.
Navigating Communication and Behavioral Changes
As dementia progresses, communication often becomes one of the biggest hurdles, leading to frustration for everyone involved. Words can get lost, sentences become jumbled, and simple intentions are easily misunderstood. But it's in these moments that real connection matters most, shifting the focus from perfect grammar to patient understanding. Providing effective home care for seniors with dementia means learning a new language—one built on patience, simple cues, and a whole lot of empathy.
At the heart of it all is remembering that the person you love is still there, even if their ability to express themselves has changed. They are trying to connect; our job is to meet them where they are. This usually means simplifying our own language and paying much closer attention to what isn't being said.
Speaking Their Language
When you're talking with a loved one with dementia, less is almost always more. Long, complex sentences can be completely overwhelming and impossible for them to process. The goal is to make your messages clear, calm, and easy to follow.
- Use Short, Simple Sentences: Stick to one idea at a time. Instead of saying, "Let's get your shoes on so we can go out to the garden before it gets too hot," try breaking it down. "It's a lovely day." (Pause.) "Let's put on your shoes." (Pause.) "We can go to the garden."
- Speak Slowly and Clearly: Use a gentle, reassuring tone. Your mood and energy are contagious, and a calm voice can help de-escalate potential anxiety before it even starts.
- Offer Simple Choices: To help them keep a sense of control, offer simple, visual choices. Holding up two different shirts and asking, "Would you like the blue or the green?" is far more effective than an open-ended question like, "What do you want to wear?"
Beyond your words, your body language is a powerful tool. Making eye contact, smiling, and using a gentle touch can communicate warmth and safety in a way words sometimes can't. To dive deeper into specific techniques, our guide on communicating with dementia patients offers more detailed strategies.
Understanding and Responding to Behavioral Changes
Challenging behaviors like agitation, repetition, or sundowning are almost always a form of communication. They aren't random acts of defiance; they're expressions of an unmet need. The person might be in pain, bored, scared, or overwhelmed. Our job as caregivers is to become detectives, looking for the root cause behind the action.
Behavior is a language. Instead of reacting to the behavior itself, try to understand what your loved one is trying to tell you. This shift in perspective transforms you from a manager of symptoms to a compassionate problem-solver.
For instance, if your mother begins pacing agitatedly every afternoon, this "sundowning" could be triggered by fatigue or the shifting light. Instead of just telling her to sit down, you could try redirecting that energy. A gentle suggestion like, "Mom, would you help me fold these towels?" can provide a soothing, purposeful activity that calms her restlessness.
Sometimes, the need is purely physical. Someone who repeatedly tugs at their pants might not be acting out—they may simply need to use the restroom. A person who refuses to eat could have dental pain. It’s always a good idea to consider physical discomfort first before assuming a behavior is purely psychological. For those providing professional support, resources offering essential care tips for working with dementia patients can be an incredible help in this process.
A Proactive Approach to Difficult Moments
It's always better to prevent a difficult situation than to de-escalate one. Once you start to understand your loved one's triggers and daily rhythms, you can proactively create a calming environment that minimizes stress.
- Validate Their Feelings: If they're upset because they think they need to go to work, arguing that they're retired will only increase their distress. Instead, join them in their reality. "It sounds like you're worried about work today. You were always so dedicated."
- Redirect with a Positive Activity: After validating, gently pivot to something pleasant and familiar. "Before you go, could you help me with this puzzle? I can't seem to figure it out."
- Maintain a Calm Environment: Reduce background noise from TVs or radios, which can be overstimulating. A quiet, predictable space helps prevent the kind of sensory overload that can lead to agitation.
By responding with compassion and looking for the need behind the behavior, you can navigate these changes with much more confidence. This approach not only resolves difficult moments more effectively but also strengthens the loving bond between you and your loved one.
Getting Help With Professional Care and NJ Medicaid
Caring for a loved one with dementia is a profound act of love, but it’s a journey you don’t have to—and shouldn’t—walk alone. Deciding you need professional support isn't a sign of failure; it’s a sign of wisdom. Bringing in a trained caregiver can dramatically improve your loved one’s safety and quality of life while giving you the essential break you deserve.
Of course, the next logical question for many families in Mercer County is a practical one: how do we pay for it? The financial side of care can feel just as overwhelming as the emotional side. The good news is that for many New Jersey residents, programs like Medicaid are a critical lifeline, making high-quality home care for seniors with dementia an accessible reality.
Finding the Right In-Home Care Provider
When you start looking for an in-home care agency in towns like Princeton or Hamilton, you’re searching for more than just a service—you’re looking for a partner. This partnership has to be built on trust, skill, and genuine compassion. Your first step should be to find agencies that truly specialize in dementia care, because it requires very specific training and a unique approach.
During the interview process, dig deeper than the basic questions about services and costs. You need to understand how they handle the specific, day-to-day challenges of dementia.
- What is their caregiver training like? Ask if their aides are specifically trained in dementia communication, behavior management, and safety protocols. Don't be shy about asking for details.
- How do they handle caregiver consistency? Will your loved one see a familiar face each day, or will it be a revolving door of new people? A steady, trusted presence is vital for someone with dementia.
- What's their approach to challenging behaviors? Ask for real-world examples. "How would your caregiver handle a situation where my mom is agitated in the evening and refusing to get ready for bed?"
A quality agency will not only welcome these questions but will provide clear, confident answers. They should feel like a resource and an ally from your very first conversation.
The flowchart below shows a simple but effective framework that our trained caregivers use to respond to dementia-related behaviors. The key is to look for the underlying need.
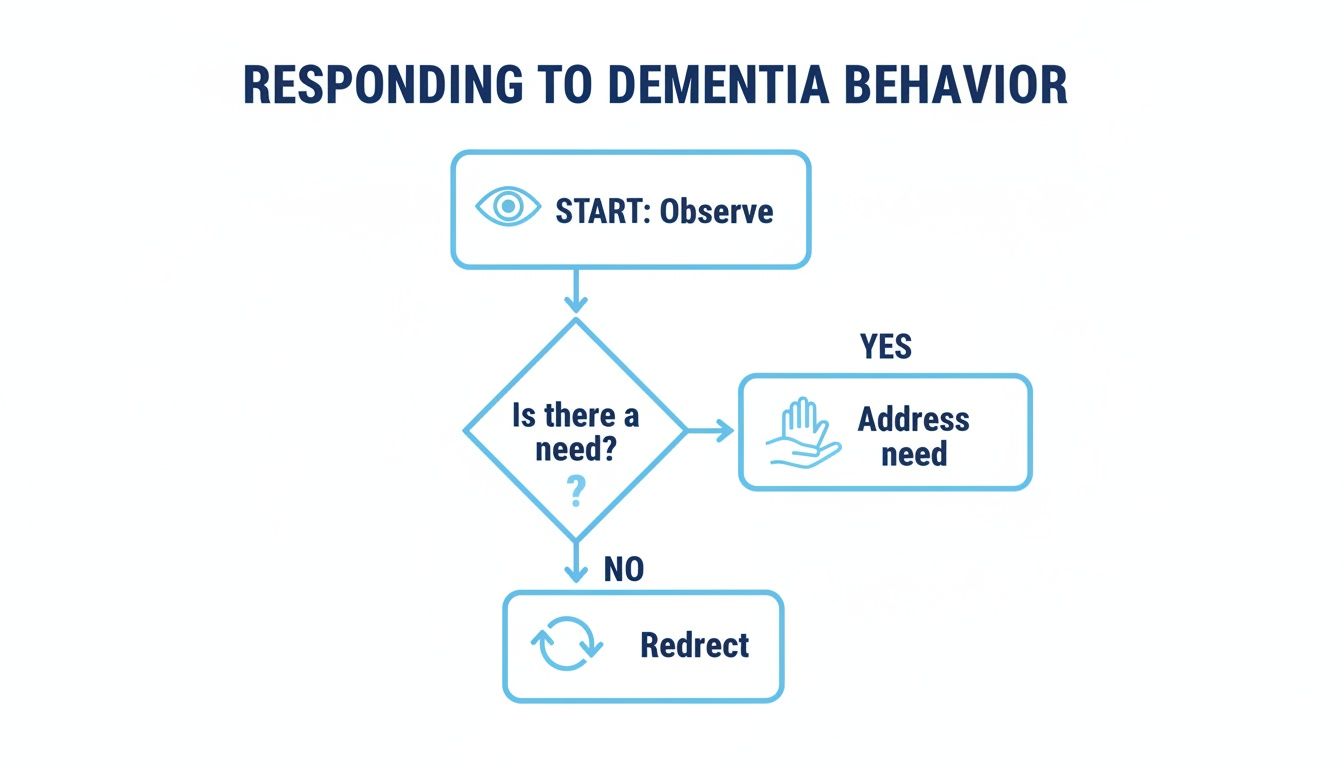
This process reminds us that behavior is often a form of communication. Instead of just reacting to the action, the goal is to address the root cause—be it pain, fear, hunger, or confusion.
Making Care Affordable with NJ Medicaid
Let's be honest: the financial burden of dementia care is staggering. The global economic cost soared past $1.3 trillion back in 2019, and a huge portion of that falls on the shoulders of unpaid family caregivers. In the U.S., families often face massive out-of-pocket costs, which makes publicly funded programs absolutely essential. You can find more details on the global costs of dementia care on Yale's website.
This is where New Jersey Medicaid can make a life-changing difference. The program designed to help is called Managed Long-Term Services and Supports (MLTSS). It’s set up to help eligible seniors get the care they need right in their own homes, avoiding a nursing facility. This program can cover a wide range of services, including the personal care assistance you’d get from a home care agency.
Navigating Medicaid can seem complicated, but its purpose is simple: to ensure that vulnerable seniors have access to the care they need to live safely and with dignity at home. Don't let the paperwork intimidate you from exploring this powerful resource.
Eligibility for NJ Medicaid and the MLTSS program boils down to two main factors: medical need and financial status.
- Medical Need: The applicant must require a nursing-home level of care. For someone with dementia, this is usually determined by their need for help with Activities of Daily Living (ADLs) like bathing, dressing, and mobility, or because they need constant supervision to stay safe.
- Financial Status: There are strict income and asset limits. As of 2024, an individual generally must have a very limited monthly income and few countable assets to qualify.
NJ Medicaid Home Care Eligibility Checklist (Simplified)
Applying for Medicaid can feel like navigating a maze. This simplified table breaks down the core requirements for programs like MLTSS in New Jersey to give you a clearer starting point.
| Eligibility Area | General Requirement (Mercer County) | Where to Get Help |
|---|---|---|
| Medical Need | Must require a "nursing facility level of care," often meaning significant help with ADLs or supervision due to cognitive impairment. | Your loved one's doctor can provide a medical assessment. A Medicaid-approved home care agency can also help evaluate needs. |
| Monthly Income | Income must be below a specific threshold (this amount changes annually). For 2024, it's generally under $2,829 for an individual. | Mercer County Board of Social Services or an elder law attorney can provide the exact, current figures and explain what counts as income. |
| Total Assets | Countable assets must be very low, typically $2,000 or less for an individual. Some assets, like a primary home, are often exempt. | An elder law attorney is the best resource for understanding complex asset rules, spend-down strategies, and exemptions. |
It's important to remember that the rules are intricate and have many exceptions. Many families find it helpful to get expert guidance when applying.
For a much more detailed breakdown, you can learn about the different NJ Medicaid waiver programs and their specific requirements to see how they might help your family. Partnering with a Medicaid-approved agency like NJ Caregiving can also simplify things, as we can help you understand the steps and make sure you have the right documentation ready to go.
Protecting Your Own Wellbeing as a Caregiver

Providing effective home care for seniors with dementia draws on an incredible reserve of patience, empathy, and energy. It's a role that can be profoundly rewarding, but it’s also physically and emotionally draining. The most critical part of a sustainable care plan—and the one that often gets ignored—is protecting your own health.
You simply cannot pour from an empty cup. Pushing your own needs aside doesn't make you a better caregiver; it's a direct path to burnout. That state of total emotional, physical, and mental exhaustion can compromise the very care you're trying to provide.
Recognizing the Signs of Caregiver Burnout
Burnout is sneaky. It doesn't show up one morning; it creeps in over weeks and months, often starting with just feeling tired all the time. It’s crucial to pay attention to these common red flags in yourself or other family caregivers:
- Social withdrawal: You start turning down invitations from friends or feel you’ve lost interest in hobbies you used to love.
- Changes in sleep patterns: This isn’t just one bad night. It’s consistent trouble falling asleep, or maybe you’re sleeping far more than you used to.
- Increased irritability: You find yourself with a much shorter fuse, feeling angry or even resentful toward your loved one and others.
- Feeling hopeless or overwhelmed: A persistent sense that you're trapped or that nothing you do really makes a difference.
If any of this sounds familiar, it's a clear signal that you need more support. You are not alone in this. In the U.S., nearly 12 million family members provide an estimated 19.2 billion hours of unpaid care each year to loved ones with dementia. A recent analysis found that almost 60% of these caregivers have at least one modifiable health risk, like hypertension, highlighting the physical toll this role can take. You can learn more about the challenges dementia caregivers face in this report.
The Lifeline of Respite Care
This is where respite care becomes a true lifeline. Simply put, respite care is a short-term break for you. It’s not a luxury—it’s an absolute necessity for your health and your ability to continue providing quality care.
Taking time for yourself is a critical part of the care plan. It allows you to recharge, focus on your own life, and return to your caregiving role with renewed energy and perspective.
Professional respite services, like those offered by NJ Caregiving, can have a trained caregiver step in for a few hours, a full day, or even longer. This gives you a guaranteed block of time to run errands, see your own doctor, connect with friends, or just rest without feeling like you have to be "on."
Building a support system is just as crucial. This might mean setting up a regular check-in call with a sibling, finding a local caregiver support group in Mercer County, or just being honest with friends about what you're going through. You don't have to carry this weight by yourself. Prioritizing your wellbeing is the only way to ensure you can be there for your loved one in a healthy, sustainable way.
Your Dementia Home Care Questions Answered
When you're navigating the complexities of home care for a loved one with dementia, a lot of questions come up. It's completely natural. Families in Mercer County just want to feel confident they're making the best decisions, and getting clear, straightforward answers is the first step.
Let's walk through some of the most common concerns we hear from families just like yours.
How Do I Know It's Time for Professional Help?
This is the big one, isn't it? Wondering if you're hitting your limit is a thought that crosses every family caregiver's mind. The truth is, the "right" time often announces itself through a few key signs.
Maybe you're feeling completely burned out, and your stress levels are through the roof. Or perhaps you're growing more concerned about safety—a recent fall, a close call with the stove, or an instance of wandering. Sometimes it's more subtle, like a noticeable decline in personal hygiene or realizing their medical needs have become too complex for you to handle alone.
Key Takeaway: Bringing in professional help isn't a sign of failure. It’s a loving and proactive decision to ensure your family member gets the best possible care while protecting your own well-being.
What’s the Difference Between Companionship and Personal Care?
It’s easy to get these terms mixed up, but knowing the difference helps you find exactly the right kind of support.
Companionship care is all about social and emotional well-being. Think of it as having a friendly face to share stories with, play a game of cards, or just provide a safe and reassuring presence. This is huge for combating the loneliness and isolation that can come with dementia.
Personal care is more hands-on. This involves direct assistance with what we call Activities of Daily Living (ADLs)—things like bathing, dressing, grooming, and help with moving around safely.
For most people living with dementia, the best support is a thoughtful combination of both. They need that human connection just as much as they need help with the physical tasks of the day.
At NJ Caregiving, we've helped countless families figure out these next steps. If you want to talk through your specific situation and learn more about our specialized dementia care in Princeton and the surrounding communities, you can find us at https://njcaregiving.com.


