Stepping into the role of a caregiver for someone with congestive heart failure (CHF) is a profound act of love, but it's a journey you don't have to walk alone. Think of congestive heart failure home care as a partnership between you, your loved one, and their healthcare team. Success really comes down to creating a consistent daily rhythm of monitoring weight, managing medications, and catching subtle symptoms before they turn into emergencies.
Your Foundational Role in CHF Home Care
Caring for a person with congestive heart failure at home is an immense responsibility, one that blends compassion with a bit of clinical diligence. Your observations and actions have a direct, daily impact on their stability and well-being. This guide is here to be your partner in that process, breaking down complex medical advice into simple, manageable actions you can take every day.
The reality is, CHF is a massive and growing health concern. It's reached near-epidemic levels, with roughly 6.7 million Americans over the age of 20 currently living with the condition. When you become a caregiver, you join a huge, often unseen, network of people dedicated to this work. You can get a clearer picture of these numbers by reading this overview of heart failure statistics.
To keep things from feeling overwhelming, it helps to organize your efforts around a few core pillars. These are the essentials that give structure to your day and help prevent a crisis before it starts.
For a quick overview, here are the core tasks that form the foundation of successful CHF home care.
The Four Pillars of Daily CHF Home Care
| Care Pillar | Daily Action | Why It Matters |
|---|---|---|
| Daily Monitoring | Weigh them at the same time each morning. Check for swelling in feet, ankles, and legs. | This is your early warning system. Sudden weight gain is the #1 sign of fluid retention, a primary danger in CHF. |
| Medication & Diet | Administer all medications exactly as prescribed. Stick to low-sodium and fluid-restricted diets. | Consistency is everything. This prevents symptom flare-ups and keeps blood pressure and fluid levels stable. |
| Symptom Recognition | Watch for subtle changes like new shortness of breath, increased fatigue, or a persistent cough. | You are the frontline observer. Catching these small changes early allows the doctor to intervene before it requires a hospital visit. |
| Supportive Environment | Ensure the home is safe and clutter-free. Encourage gentle movement and provide crucial emotional support. | This goes beyond medicine. A safe, calm environment reduces stress on the body and mind, promoting overall well-being. |
Mastering these four areas is the key to providing excellent care and giving both you and your loved one peace of mind.
A study on home-based care found that when family caregivers are supported by formal care providers, patients report better health, higher mobility, and a lower likelihood of depression compared to receiving family care alone. It really highlights the power of having a team approach.
This guide will walk you through each of these pillars, offering practical steps and real-world advice to build your confidence and help you provide exceptional congestive heart failure home care.
Mastering Daily Monitoring to Prevent Emergencies
When you’re caring for someone with congestive heart failure, consistent daily monitoring is your single most powerful tool. Think of it as an early warning system. A simple, predictable routine can help you spot fluid retention or other brewing issues long before they turn into a full-blown medical crisis.
This isn’t about becoming a medical expert overnight. It's about paying close, careful attention to a few key signals every single day.
The reality is, heart failure is a serious condition, contributing to 9.3% of all cardiovascular disease deaths in the U.S. And with a staggering 71.0% of out-of-hospital cardiac arrests happening at home, the role you play as a caregiver is absolutely vital in preventing these emergencies. For a deeper dive into the numbers, the ACC provides extensive data on the impact of heart failure.
The Daily Weigh-In Ritual
If you do one thing every day, make it this: the daily weigh-in. A sudden jump on the scale is the number one sign that the body is holding onto extra fluid, which puts immense strain on an already struggling heart. For this to work, it has to be done the same way, every time.
Here's the routine we teach families:
- Same Time, Every Time: First thing in the morning is best, right after using the bathroom and before eating or drinking anything.
- Same Scale, Same Spot: Use the exact same digital scale on a hard, flat surface. No carpet!
- Same Clothes (or None): Have them wear the same lightweight pajamas or nothing at all. Consistency is everything.
- Log It Immediately: Don't rely on memory. Write the number down in a dedicated notebook or a tracking app on your phone right away.
A sudden gain of more than two to three pounds in one day, or five pounds over a week, is a major red flag. This isn't normal weight fluctuation; it's fluid. It means you need to call their doctor.
This simple habit provides the hard data doctors need. Someone might not feel much different, but the scale doesn’t lie. It can reveal a problem that’s just getting started. This kind of proactive tracking is a cornerstone of our work in reducing hospital readmissions for seniors.
This flowchart breaks down the four pillars of daily CHF management, showing how monitoring, medications, diet, and symptom awareness all fit together.
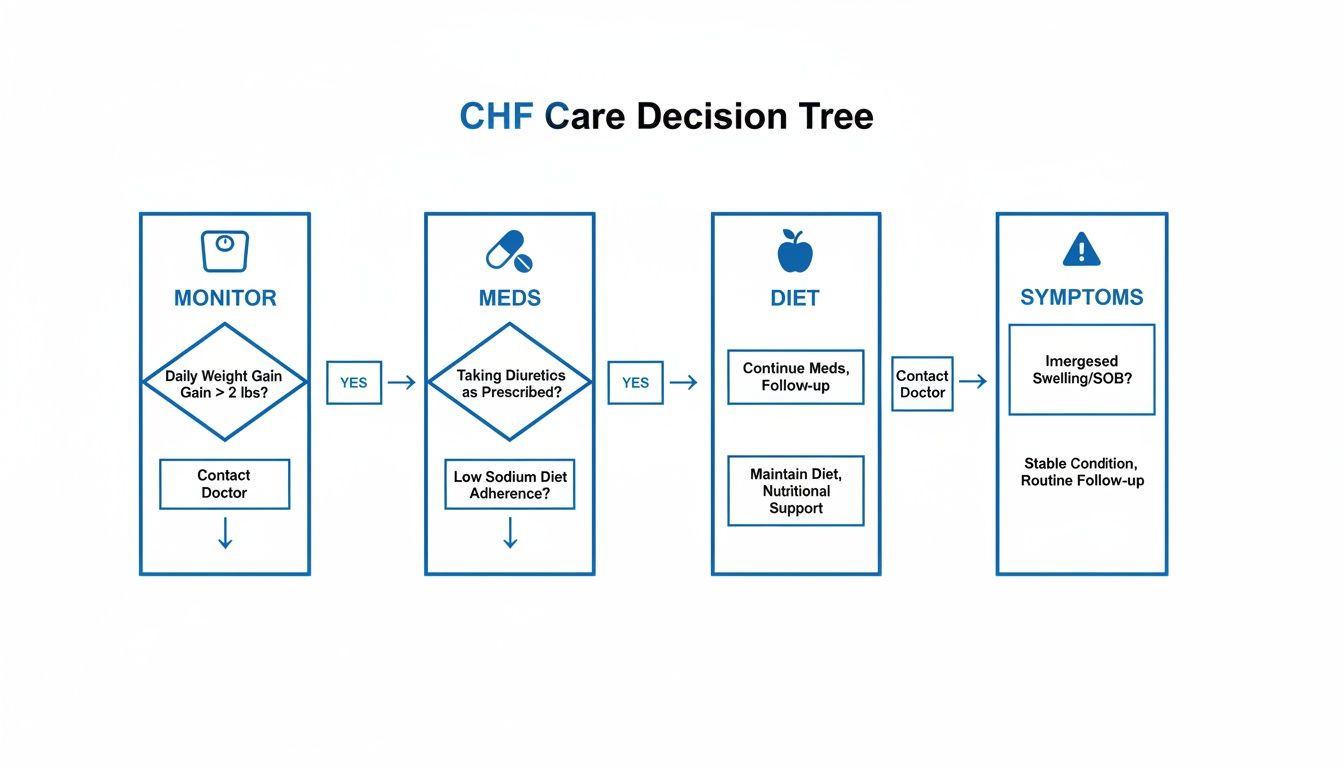
As you can see, each piece informs the next, creating a cycle of proactive care that keeps you ahead of a potential crisis.
Checking for Swelling and Other Key Symptoms
Beyond the scale, your own eyes and ears are incredibly important. The fluid that shows up as weight gain also likes to pool in specific parts of the body. This is called edema.
Make these quick checks part of your daily routine:
- Look at the Legs and Ankles: Gently press your thumb into the skin on their shin or the top of their foot for a few seconds. If a little dent or "pit" remains after you lift your thumb, that's called pitting edema.
- Listen to Their Breathing: When they’re resting, do they sound breathless? Do you hear any faint crackling or "wet" sounds?
- Ask About Their Sleep: A classic sign of worsening CHF is needing to prop up on more pillows to breathe comfortably at night. Ask them, "How many pillows did you use last night?"
- Gauge Their Energy: Is their fatigue noticeably worse than yesterday? Unexplained, heavy exhaustion can mean the heart is working way too hard.
Knowing When to Call for Help
Gathering all this information is half the battle; the other half is knowing what to do with it. The good news is that not every change is an emergency. Having a clear plan removes the anxiety and guesswork.
We created this simple guide to help caregivers know exactly what to do based on the symptoms they see.
CHF Symptom Response Plan
| Symptom Level | What to Look For | Your Next Step |
|---|---|---|
| Monitor & Log | Minor tiredness, slight swelling that's gone by morning, stable weight. | Keep up your daily routine. Make a note of these small changes in your log to discuss at the next doctor's visit. |
| Call the Doctor | Weight gain of 2-3 lbs in 24 hours, new or worse swelling in the legs, a nagging dry cough, needing extra pillows to sleep. | Call their doctor's office during business hours. Don't wait. They can often adjust medications right over the phone. |
| Call 911 | Severe shortness of breath, any chest pain or pressure, sudden confusion or fainting, coughing up pink or foamy liquid. | Do not hesitate. This is a medical emergency. Call 911 immediately. |
Having this plan handy can give you confidence and help you act quickly and appropriately, ensuring your loved one gets the right level of care at the right time.
A Practical Approach to Diet, Fluids, and Medication
Let's be honest: managing the delicate balance of medications, a low-sodium diet, and fluid restrictions can feel like the toughest part of congestive heart failure home care. It’s a constant tightrope walk. But with a few real-world strategies, you can turn these complex rules into a simple, manageable daily routine.

Streamlining Medication Management
The medication list for CHF can be long and complicated, with different pills at different times. Consistency is everything here, and some simple tools can make all the difference. A weekly pill organizer isn't just a suggestion; it's a necessity. It gives you an instant visual check to confirm if meds have been taken.
To create a nearly foolproof system, pair that organizer with technology. Set recurring daily alarms on a smartphone or smart speaker for every dose. Don't just set a generic alarm—label it with the specific medication, like "Take Lasix now" or "Time for Beta-Blocker." This takes the guesswork out of the equation.
It also really helps to know why each medication is so important:
- Diuretics (Water Pills): These are the workhorses that help the kidneys flush out extra salt and water. This reduces fluid buildup and makes it easier for the heart to do its job.
- ACE Inhibitors/ARBs: Think of these as relaxers for the blood vessels. They lower blood pressure, which means the heart doesn't have to work as hard.
- Beta-Blockers: These slow the heart rate and lower blood pressure, helping the heart pump more efficiently and with less strain.
If the sheer number of prescriptions feels like too much to handle, professional support might be the next step. Looking into senior medication management services can open up options for ensuring everything is taken safely and correctly.
Making a Low-Sodium Diet Delicious
"Low sodium" does not have to mean "low flavor." The trick is to stop thinking about what you're taking away (salt) and start focusing on what you're adding. The standard recommendation is to stay under 2,000 milligrams of sodium per day, which means becoming a bit of a detective with food labels and cooking habits.
Put the salt shaker away and build a new flavor arsenal.
- Herbs and Spices: Stock up on salt-free powerhouses like garlic powder, onion powder, smoked paprika, cumin, and dried herbs like oregano and basil.
- Acids: A squeeze of fresh lemon or a splash of vinegar at the end of cooking brightens up dishes and gives them a tang that can mimic salt.
- Aromatics: Sautéing fresh garlic, onions, and celery is a classic way to build a deep, savory flavor base for almost any dish, no salt required.
Getting familiar with the basics of a heart-healthy diet plan is a game-changer for managing CHF at home. It empowers you to make smarter, healthier choices every time you go to the grocery store.
Caregiver Tip: Watch out for "hidden sodium." It's not just in chips. Canned soups, processed meats, frozen dinners, and even bread can be packed with salt. Always, always check the nutrition label for the sodium content and pay close attention to the serving size.
Smart Strategies for Managing Fluid Intake
Fluid restriction can be one of the most challenging adjustments. You're essentially fighting the body's natural urge to drink when thirsty. The goal is to make the limited amount of fluid feel like it's enough.
First, get the exact daily limit from the doctor. It's often around 64 ounces (2 liters), but this can vary. Remember, this total includes all liquids—water, coffee, tea, juice—and even foods that are liquid at room temperature, like soup, ice cream, and Jell-O.
Here are a few tricks we've seen work wonders:
- Use smaller cups. An 8-ounce glass that's full feels much more satisfying than a 16-ounce glass that's half-empty.
- Sip, don't gulp. Encourage slow sipping throughout the day to make the feeling of drinking last longer.
- Track it visually. Use a water bottle with measurements on the side or a simple chart on the fridge to keep a running tally.
- Soothe a dry mouth. Offer sugar-free hard candy, gum, or frozen fruit like grapes to suck on. Sometimes just rinsing the mouth with cold water (without swallowing) can provide immediate relief.
Creating a Safe and Energy-Conserving Home
For someone with congestive heart failure, fatigue isn't just about feeling tired. It's a deep, overwhelming exhaustion that can turn simple daily tasks into monumental efforts. The key is to transform their living space from a potential obstacle course into a sanctuary that conserves precious energy and minimizes risk. This isn't about huge renovations; it's about smart, small adjustments that make a world of difference.
These modifications empower them to maintain their independence and create a calming environment that truly supports their well-being. And the need for effective, practical home-based solutions is growing. The global market for congestive heart failure care was valued at nearly $25 billion in 2025 and is expected to climb to over $40 billion by 2032. These numbers underscore just how critical these at-home strategies are for improving patient outcomes. You can explore the full congestive heart failure market report to see the full picture of this trend.

Reducing Trip Hazards and Improving Lighting
First things first: clear the way for safe movement. Falls are a major risk for anyone with limited energy and mobility, but thankfully, many common hazards are surprisingly easy to fix.
Take a walk through each room, trying to see it from their perspective. Look low and scan the floors, hallways, and especially the staircases.
- Secure Rugs: Those small throw rugs are notorious for slipping. If you can't remove them completely, make sure they are anchored down with double-sided rug tape or a quality non-slip backing.
- Clear the Clutter: Piles of magazines, stray electrical cords, and other items lying around are just waiting to cause a fall. Find a home for everything.
- Brighten the Way: Good lighting is non-negotiable. Make sure hallways, stairs, and bathrooms are brightly lit. A few well-placed nightlights can make all the difference for navigating safely after dark.
Strategic Organization to Conserve Energy
Next, think like an efficiency expert. The goal is to rearrange the environment so that essential items are always within easy reach, eliminating unnecessary bending, stretching, or walking.
Consider the items your loved one uses most throughout the day. Where are they? If they're tucked away in low cabinets or high shelves, it's time to move them.
A simple but impactful change is reorganizing the kitchen. Move frequently used dishes, pans, and food items from low cabinets to the countertop or easy-to-reach shelves. This small adjustment saves energy with every meal.
This same logic applies everywhere. Put their favorite blanket, the remote control, and reading glasses in a basket right next to their chair. In the bedroom, organize their closet so that daily outfits are right at the front. It’s all about minimizing effort.
Enhancing Bathroom Safety
The bathroom is often the most high-risk room in the house, thanks to wet surfaces and the constant up-and-down movement. A few key pieces of equipment can drastically improve safety and give everyone peace of mind.
These additions are often straightforward to install but have a huge payoff. Making sure the home is safe and functional is a cornerstone of good care; you can explore a wide range of home modifications for seniors that support aging in place.
Here are the most impactful additions for the bathroom:
- Grab Bars: Install sturdy grab bars next to the toilet and inside the shower or tub. Remember, towel racks are not designed to support a person's weight.
- Shower Chair: A stable chair or bench allows them to sit while bathing, which conserves a tremendous amount of energy and reduces the risk of slipping on a wet surface.
- Raised Toilet Seat: This simple device makes it much easier to sit down and stand back up, which can be a real struggle for someone dealing with weakness and fatigue.
Coordinating With Healthcare Professionals
As the primary caregiver, you quickly become the central hub of communication—the one person connecting your loved one with their entire medical team. For congestive heart failure, keeping those lines of communication open isn't just a nice idea; it's absolutely essential. Clear, consistent updates flowing in both directions ensure everyone is working from the same playbook, which is how you prevent complications before they start.
This isn't just about being organized. It's about better outcomes. Research has shown that when professional caregivers and family members work together as a team, individuals report better health, higher mobility, and a lower likelihood of depression compared to getting family care alone. Think of it as building a support network with a single, powerful goal: improving their quality of life.
Making the Most of Doctor Visits
Doctor's appointments can feel like a whirlwind. They're often short, packed with information, and it's easy to walk out feeling like you forgot something important. The key to making every visit count is preparation. Don't try to rely on memory alone—the stress of the moment can blank your mind.
Before you go, take a few minutes to get your thoughts and observations down on paper. A simple, organized list can transform the appointment from a rushed update into a productive conversation.
- Bring Your Daily Log: That notebook with daily weights, blood pressure readings, and symptom notes is pure gold. It gives the doctor hard data to work with, not just vague feelings about how things have been going.
- List Every Question: Seriously, write them all down. Is a new side effect normal? Can you clarify a dietary restriction? No question is too small when it comes to managing CHF.
- Summarize What's Changed: Note any new or worsening symptoms. Be specific. Instead of "His breathing is worse," say, "For the past week, he's needed three pillows to sleep, up from just one."
- Have an Updated Medication List: Bring a complete list of everything they take—prescriptions, dosages, vitamins, and any over-the-counter supplements.
Caregiver Tip: Ask the doctor if you can use your phone's voice recorder during the appointment. It lets you focus completely on listening and asking questions, knowing you can review the exact details later without worrying you missed something.
The Simple Power of a Health Binder
In a crisis, the last thing you want to do is scramble for paperwork. A simple three-ring binder can become your health command center, keeping every critical piece of information in one grab-and-go spot.
Organize your binder with dividers to make things easy to find:
- Key Contacts: One page with phone numbers for all doctors, specialists, the pharmacy, and emergency contacts.
- Medication List: A current, typed list of all prescriptions, dosages, and supplements.
- Recent Test Results: Copies of recent lab work, ECGs, or imaging reports.
- Appointment Notes: A section for your notes from each visit, so you can track recommendations over time.
This binder becomes the single source of truth for your loved one’s care. Whether you're seeing a new specialist or talking to an EMT, they can get a fast, accurate picture of the medical history.
When the daily tasks start to feel overwhelming, remember you don't have to manage it all on your own. Bringing in professional in-home care can supplement your efforts, offering specialized support and giving you a much-needed break. A professional caregiver from a trusted agency like NJ Caregiving can become a valuable partner on your team, helping with medication reminders, meal prep, and daily monitoring to ensure nothing falls through the cracks.
Prioritizing Your Own Well-Being as a Caregiver
Caring for someone with congestive heart failure is a marathon, not a sprint. Your focus is naturally on your loved one, but ignoring your own well-being is the fastest way to hit a wall. Burnout doesn't help anyone, and your energy, patience, and health are the most valuable resources you have.
It's an old saying, but it's true: you can't pour from an empty cup. Taking care of yourself isn't selfish. It's an essential part of being an effective, compassionate, and sustainable caregiver for the person who depends on you.
Recognizing the Signs of Burnout
Caregiver burnout is a state of physical, emotional, and mental exhaustion that can sneak up on you. It often starts as small, subtle changes that build over time. Being honest with yourself and catching these early signs is the first step toward preventing a more serious decline.
Keep an eye out for these common red flags:
- Persistent Fatigue: A deep-seated tiredness that sleep just can't seem to fix.
- Increased Irritability: Finding yourself unusually short-tempered or resentful toward your loved one or others.
- Social Withdrawal: Losing interest in hobbies and activities you once enjoyed, or starting to avoid friends.
- Changes in Health: Noticing more frequent headaches, stomach issues, or just getting sick more often than you used to.
If any of this sounds familiar, take it as a clear signal that you need to invest in your own care. For a deeper dive into this topic, explore our guide on practical self-care for caregivers.
Building a Sustainable Self-Care Routine
Self-care doesn’t have to mean week-long vacations or expensive spa days. The most effective strategies are the small, consistent actions you weave into your daily life. The trick is to make these breaks non-negotiable.
"As a caregiver, I think it is hard to ask for and get help. Professional help could actually be beneficial to the loved one, so it isn’t necessarily selfish to share the responsibility."
Try to schedule small pockets of time just for you, even if it's only 15-20 minutes. Go for a brisk walk, listen to a podcast, or just sit quietly with a cup of tea behind a closed door. These little moments are vital for resetting your mental state.
Most importantly, learn to ask for and accept help. Reach out to friends, family members, or professional services like NJ Caregiving for respite care. Having a trusted person step in for just a few hours can give you the breathing room you need to recharge and return to your role with renewed strength and patience.
Common Questions About Congestive Heart Failure Home Care
Stepping into the role of a caregiver for someone with congestive heart failure naturally comes with a lot of questions. Getting clear, practical answers helps build your confidence so you can focus on what’s most important: providing safe and compassionate support. Let's walk through some of the most common concerns we hear from families who are just starting this journey.
What Are the Most Critical Daily Red Flags?
Your daily check-ins are your first line of defense against a potential crisis. While you’ll be tracking several symptoms, a few specific signs demand immediate attention because they point directly to fluid buildup—the biggest strain on a weakened heart.
Keep a sharp eye out for these signals:
- Sudden weight gain of more than two to three pounds in a single day, or five pounds in one week.
- Increased swelling (edema) in the legs, ankles, or stomach that's either new or clearly worse than the day before.
- Worsening shortness of breath, especially if it happens when they’re resting or trying to lie down flat.
- A new or nagging dry cough that just won't go away.
Any one of these symptoms is a reason to call their doctor's office right away. But if they experience severe chest pain, have extreme trouble breathing, or seem suddenly confused, call 911 immediately.
How Can I Make Low-Sodium Meals Taste Good?
The fear of bland, boring food is a huge hurdle for many families, but a low-sodium diet is far from a flavorless one. The trick is to stop thinking about what you're taking out (salt) and start focusing on all the flavors you can add in. Your first move? Get the salt shaker off the table for good and start building a new flavor arsenal.
The secret is flavor layering. Stock up on salt-free seasoning blends, garlic and onion powder, paprika, and fresh herbs like basil or cilantro. A simple squeeze of lemon or lime juice right before serving can brighten up an entire dish, mimicking the familiar tang of salt.
Another pro-tip is to roast vegetables instead of boiling them. This caramelizes their natural sugars and creates a deep, rich flavor you just can't get from a pot of water. With a little creativity, you’ll be shocked at how much taste you can pack into a meal without ever reaching for the salt.
Is It Safe for Someone with CHF to Exercise?
For most people with stable congestive heart failure, gentle movement isn't just safe—it's incredibly beneficial for their strength, mood, and overall quality of life. The most important step, however, is to get a clear, doctor-approved exercise plan from their cardiologist or a cardiac rehab specialist. You should never start a new activity program without their specific guidance.
Typically, the recommendation is for light to moderate movement. Think things like:
- Slow walking on a flat, even surface
- Seated leg lifts and arm circles
- Gentle stretching
The golden rule here is to start slow and listen to their body. They should stop immediately if they feel dizzy, more short of breath than usual, or have any chest discomfort. When it comes to exercise and CHF, consistency with gentle movement is always better than intensity.
Managing the daily realities of congestive heart failure care can feel overwhelming, but you are not in this alone. The dedicated team at NJ Caregiving provides professional, compassionate in-home support to help with everything from daily monitoring and meal prep to personal care, giving you and your family true peace of mind. To learn more about how we can help, visit us at https://njcaregiving.com.