Navigating Medicaid Eligibility NJ: The Essentials
Understanding Medicaid eligibility in New Jersey can feel like navigating a maze. However, access to affordable healthcare makes it a crucial journey. This section simplifies the key aspects of Medicaid eligibility in New Jersey, focusing on NJ FamilyCare, the state's Medicaid program. We'll explore different routes to coverage, highlighting how income, family size, and other factors influence eligibility.
Understanding NJ FamilyCare
NJ FamilyCare caters to a diverse population with a range of healthcare needs. It's not a uniform program. Instead, it offers various coverage options based on specific criteria. Think of it as a collection of interconnected programs, each designed for particular groups, such as children, pregnant women, parents, and adults without children. This targeted approach ensures coverage reaches those who need it most.
Income and Eligibility: The MAGI Calculation
For many applicants, income plays a crucial role in determining eligibility. New Jersey utilizes the Modified Adjusted Gross Income (MAGI) to evaluate financial eligibility for most NJ FamilyCare programs. MAGI isn't the same as your regular gross income. Certain deductions and exemptions may apply, potentially resulting in a lower MAGI than your actual income. This can be especially beneficial for individuals near the income limit. Understanding precisely what is included and excluded in the MAGI calculation is essential.
Beyond Income: Categorical Eligibility
While income is often the first step, New Jersey's Medicaid eligibility also considers categorical eligibility. This means certain groups automatically qualify for coverage regardless of income. Pregnant women and children often fall into specific categorical eligibility groups. This simplifies the application process for individuals facing unique circumstances.
As of October 2024, approximately 1,753,610 New Jersey residents were covered by Medicaid and CHIP through the NJ FamilyCare program. This illustrates the program's significant reach. Medicaid expansion under the Affordable Care Act (ACA) significantly boosted this increased coverage. Find more detailed statistics here. This expansion, along with policy changes like the Cover All Kids initiative, shows New Jersey's dedication to providing accessible healthcare. For instance, expanding children's eligibility regardless of immigration status marks a substantial step towards inclusivity. These efforts highlight the state's proactive stance on ensuring healthcare coverage for its residents.
Breaking Down Income Requirements That Actually Matter
Income limits are crucial when determining Medicaid eligibility in New Jersey, but the process can be confusing. This section clarifies how income affects your chances of qualifying for NJ FamilyCare. It's more than just looking at your annual salary.
How New Jersey Calculates Income for Medicaid
New Jersey uses the Modified Adjusted Gross Income (MAGI) method for most Medicaid applicants. MAGI provides a tailored view of your income. It's similar to the Adjusted Gross Income (AGI) used for taxes, but with key differences for Medicaid. Some income sources, like child support received, are excluded, and certain deductions are allowed, potentially lowering your MAGI and improving your eligibility.
Income Limits Vary by Group
Medicaid eligibility in New Jersey isn't universal. Income limits depend on factors like age, family size, and household makeup. A single adult might have different income limits than a parent with two children. Pregnant women often have higher income limits than non-pregnant adults. This tiered system aims to address the diverse financial realities of different groups.
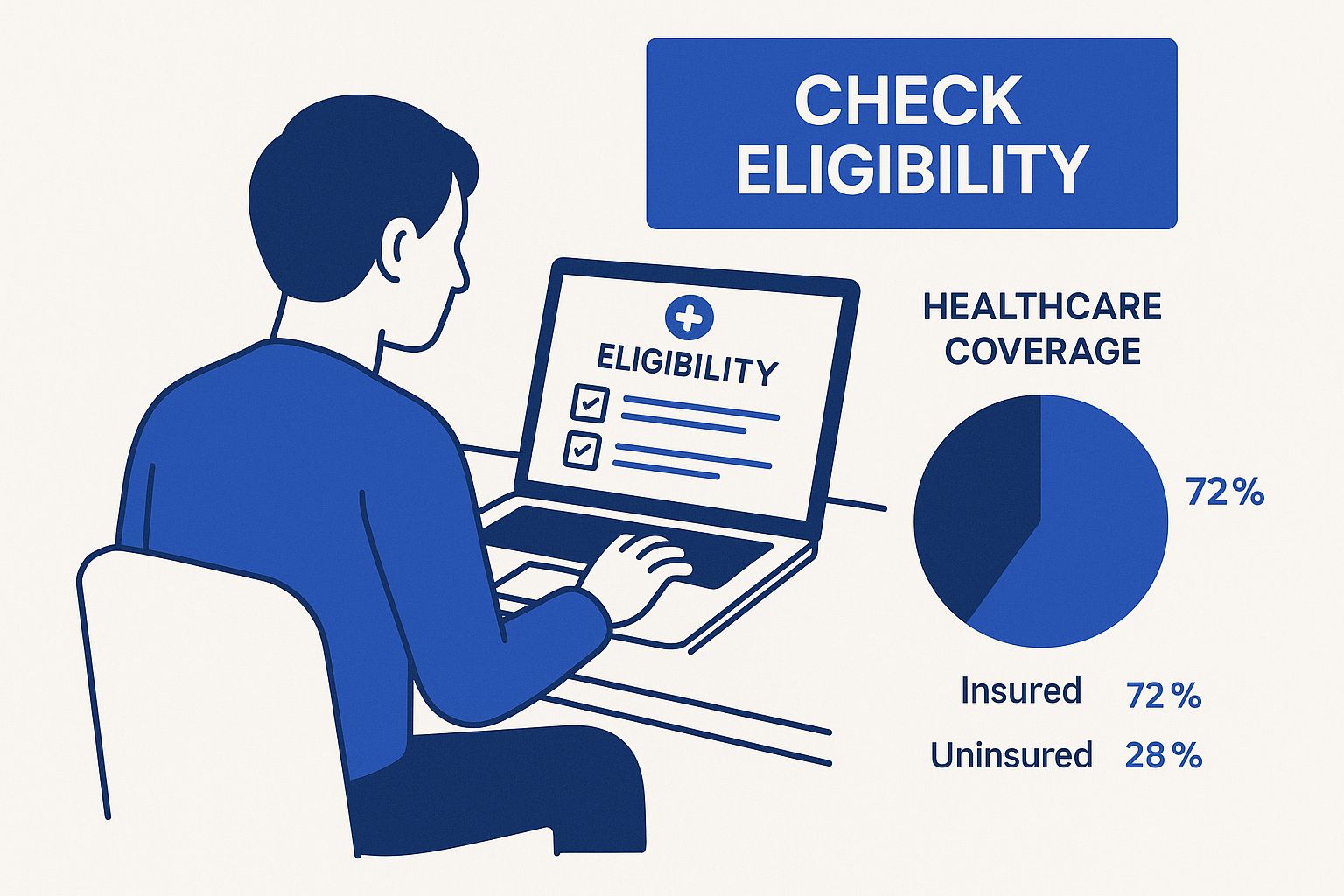
The infographic above shows someone checking their healthcare eligibility, emphasizing the importance of this first step. It highlights available online resources to simplify the process. Understanding your options is key when navigating Medicaid eligibility. You can also explore other options, like affordable health insurance.
Beyond MAGI: Other Income Considerations
While MAGI is the primary method for most, some groups are assessed differently. Seniors, blind individuals, and people with disabilities may have different income and asset limits. These alternative methods recognize their unique financial circumstances. Even if your MAGI is above the standard limit, you might still qualify based on your situation.
Asset Limits for Certain Applicants
Some NJ FamilyCare programs, particularly those for seniors, blind individuals, and people with disabilities, also consider asset limits. This means the value of your assets – like savings accounts, investments, and property (excluding your primary residence) – is considered, along with your income. However, some assets are often exempt, such as a car and a small amount of burial funds. These exemptions help individuals maintain some financial security while receiving healthcare coverage.
To help clarify income eligibility further, the following table provides a general overview of income limits for different categories within the NJ Medicaid program. Please note these are subject to change and it's always best to verify with official sources.
NJ Medicaid Income Eligibility Limits by Category
| Eligibility Category | Maximum Income (% of FPL) | Monthly Income Limit (Individual) | Monthly Income Limit (Family of 4) |
|---|---|---|---|
| Pregnant Women | |||
| Children under 19 | |||
| Parents/Caretaker Relatives | |||
| Adults (aged 19-64) | |||
| Seniors & Individuals with Disabilities |
This table shows the maximum income limits as a percentage of Federal Poverty Level (FPL) for different eligibility categories in New Jersey's Medicaid program.
This table offers a quick reference for understanding how income limits can vary. For the most accurate and up-to-date information, it is always recommended to consult the official NJ FamilyCare website or speak with a benefits specialist.
Who Qualifies: Population-Specific Pathways to Coverage
Beyond income requirements, your personal circumstances in New Jersey significantly influence your Medicaid eligibility. This section explores the various pathways to coverage under NJ FamilyCare, offering insights that can help you determine the best route to access the healthcare you need.
Children's Coverage: A Focus on Comprehensive Care
New Jersey prioritizes children's health, offering comprehensive coverage through NJ FamilyCare, including the Children's Health Insurance Program (CHIP). This program extends coverage to children in families with incomes up to 350% of the Federal Poverty Level (FPL), one of the highest thresholds in the nation.
Additionally, New Jersey's Cover All Kids initiative removed CHIP premiums and waiting periods, further simplifying access. This means quicker and more affordable healthcare for eligible children.
Coverage for Pregnant Women: Expedited Options and Extended Care
Expectant mothers have access to expedited Medicaid coverage in New Jersey. NJ FamilyCare offers coverage for pregnant women with incomes up to 200% of the FPL.
This coverage extends for 12 months after the baby's birth, ensuring continued care for both mother and child during the postpartum period. Moreover, presumptive eligibility allows pregnant women to receive immediate temporary coverage while their full application is processed.
Parents and Caretakers: Supporting Family Well-being
NJ FamilyCare also provides coverage for parents and caretakers. Eligibility for this group is income-based and tied to their role in caring for dependent children.
This pathway recognizes the importance of ensuring caregivers have access to healthcare to effectively support their families’ overall health and well-being.
Adults Without Dependents: Expanding Access to Healthcare
New Jersey expanded Medicaid eligibility to include adults without dependent children through the Affordable Care Act. Adults under 65 with incomes up to 138% of the FPL now qualify for coverage.
This expansion significantly broadened access to healthcare for a previously uninsured population segment. New Jersey's Medicaid eligibility criteria reflect the state's commitment to providing accessible healthcare, balancing federal guidelines with local needs. Historically, eligibility was tied to welfare, but the Affordable Care Act broadened access considerably. Learn more about New Jersey Medicaid's evolution.
Special Situations and Targeted Programs
NJ FamilyCare also addresses specific circumstances. Emergency Medicaid is available for non-citizens needing urgent medical care, regardless of immigration status. Targeted programs exist for individuals with specific health conditions, like breast and cervical cancer.
These programs offer crucial support to those facing significant health challenges. These policies, including the removal of immigration barriers for children's coverage in 2023, reflect New Jersey's focus on inclusive healthcare access. You might be interested in: our sitemap of categories which includes valuable information about senior care resources.

Mastering The Application Process: Start To Finish
Applying for Medicaid in New Jersey doesn't have to be a daunting task. This section provides a step-by-step guide to navigating NJ FamilyCare, offering practical advice and helpful resources.
Choosing Your Application Method
NJ FamilyCare offers various application methods, catering to individual preferences and comfort levels with technology. Each method has its own benefits:
- Online: The NJ FamilyCare online portal offers convenient, 24/7 access, often the quickest application route.
- Paper Application: Downloadable paper applications are a traditional option. Keep in mind, processing times may be longer than online submissions.
- Phone Enrollment: Enrolling by phone provides personalized assistance from a representative who can guide you through the process. This is especially helpful for those with specific questions.
- In-Person Assistance: County welfare agencies offer in-person support, perfect for those who prefer face-to-face guidance and immediate clarification.
- Certified Application Counselors: These trained professionals provide free assistance, helping gather necessary documentation and ensuring accurate application completion.
Gathering The Necessary Documentation
Having the correct documents is essential for a smooth application. Before you begin, gather these commonly required items:
- Proof of Identity: This could include a driver's license, state ID, passport, or birth certificate.
- Proof of Residency: Examples include a utility bill, lease agreement, or mail displaying your name and address.
- Proof of Income: Gather pay stubs, tax returns, or bank statements.
- Citizenship/Immigration Status (if applicable): This might involve a green card, naturalization papers, or other relevant documents. For more information, check out this helpful guide: How to master the application process
To help organize your documents, refer to the table below:
To simplify the document gathering process, we've compiled a table outlining the necessary documentation for a New Jersey Medicaid application.
Documents Needed for NJ Medicaid Application
| Document Type | Examples | Where to Obtain | Notes |
|---|---|---|---|
| Proof of Identity | Driver's license, State ID, Passport, Birth Certificate | DMV, State issuing agency, U.S. Department of State, Vital Records Office | Ensure the document is current and valid. |
| Proof of Residency | Utility bill, Lease agreement, Bank statement, Mail with your name and address | Utility company, Landlord, Bank, Post Office | The document should clearly show your current address. |
| Proof of Income | Pay stubs, Tax returns, W-2 forms, Bank statements | Employer, IRS, Bank | Provide documentation for all sources of income. |
| Citizenship/Immigration Status (if applicable) | Green card, Naturalization papers, US Passport | U.S. Citizenship and Immigration Services | Only required for non-citizens. |
This table provides a clear overview of the typical documents needed. Remember, specific requirements might vary depending on individual circumstances.
Submitting Your Application And Following Up
Once your application is complete and you've gathered all necessary documents, accurate and efficient submission is key. Follow the specific instructions for your chosen method (online, mail, or in-person). Make copies of everything for your records.
After submitting, regularly monitor your application status. NJ FamilyCare offers online and phone tracking options. Staying proactive ensures you're informed about the progress and can address any delays or requests for additional information promptly.
Troubleshooting And Seeking Assistance
Encountering issues? Don't worry! NJ FamilyCare offers various support channels. Contact their helpline or seek guidance from certified application counselors for help with common roadblocks and answers to your questions.
Understanding Timelines And Coverage
Application processing times vary, so patience is important. NJ FamilyCare strives for efficient processing. Retroactive coverage may be available in some cases, meaning coverage could apply to medical expenses incurred before approval. Understanding these timelines and coverage options helps manage expectations and ensure access to necessary care.
Post-Pandemic Medicaid Eligibility: What's Changed
The COVID-19 pandemic significantly impacted the Medicaid landscape in New Jersey. Understanding these shifts is crucial for anyone navigating Medicaid eligibility in the state. This section explains how the pandemic reshaped eligibility, highlighting the transition from the public health emergency to the current "unwinding" period.
The Continuous Coverage Provision: A Lifeline During the Pandemic
The federal Families First Coronavirus Response Act, enacted in March 2020, mandated states to maintain continuous Medicaid coverage throughout the public health emergency. In return, states received increased federal funding. New Jersey complied, halting disenrollments. Even if your circumstances changed and you typically would have lost eligibility, you remained covered. This continuous coverage provision offered vital protection during uncertain times.
The Unwinding of Continuous Coverage: What It Means For You
This period of continuous coverage eventually ended. By mid-2023, New Jersey reinstated eligibility redeterminations. This "unwinding" process reviews the eligibility of all Medicaid beneficiaries. The COVID-19 pandemic dramatically altered Medicaid enrollment in New Jersey. The Families First Coronavirus Response Act required continuous coverage during the public health emergency. New Jersey suspended disenrollments, leading to a surge in enrollment and creating reporting inconsistencies as data collection adapted. By mid-2023, redeterminations resumed, and approximately 701,320 residents were disenrolled. Explore this topic further. Address verification is a key step in applying. Learn more about address verification.
Navigating Redeterminations: Maintaining Your Coverage
If you're currently enrolled in Medicaid, understanding the redetermination process is critical. You will receive a renewal packet from NJ FamilyCare. Completing and returning this packet promptly is essential to avoid a lapse in coverage. The packet requests updated details about your household, income, and any other significant changes. For additional resources, you might be interested in this sitemap.
What If You No Longer Qualify? Exploring Your Options
If the redetermination process finds you no longer meet the requirements for Medicaid eligibility in New Jersey, you still have choices. You might be eligible for subsidized health insurance via the Affordable Care Act (ACA) Marketplace. Navigating this transition can be challenging. Assistance from an enrollment specialist or certified application counselor can be incredibly helpful in exploring alternative coverage options and ensuring continued access to necessary healthcare.
Beyond Basic Coverage: Specialized Programs That Matter
Standard Medicaid coverage in New Jersey provides a significant safety net, but it doesn't always address every individual's unique needs. For those requiring specialized care, New Jersey offers programs that go above and beyond basic Medicaid benefits, significantly improving quality of life. Let's explore these essential programs.
Managed Long-Term Services and Supports (MLTSS)
For individuals needing ongoing assistance with daily tasks, New Jersey's Managed Long-Term Services and Supports (MLTSS) program provides comprehensive care and support. The program focuses on helping individuals remain within their homes and communities, offering access to services like personal care, home health aides, and assistive devices. MLTSS is vital for maintaining independence and quality of life for those requiring consistent, long-term support.
Qualified Income Trusts (Miller Trusts)
Sometimes, income can surpass Medicaid limits, even with substantial medical needs. Qualified Income Trusts (QITs), also called Miller Trusts, provide a solution for those needing nursing home care but whose income exceeds Medicaid limits. QITs help individuals allocate income towards specific expenses, ensuring access to necessary care without undue financial strain. This can be invaluable for managing the costs of long-term care.
Home and Community-Based Services (HCBS) Waivers
Home and Community-Based Services (HCBS) Waivers offer an alternative to institutional care, expanding Medicaid eligibility in New Jersey. These waivers deliver a flexible range of services in the home or community setting, including options like personal care, respite care, and home modifications. HCBS waivers are especially beneficial for individuals wanting to maintain independence and community ties while receiving essential care.
Medicare-Medicaid Dual Eligibles: Coordinating Benefits
Navigating benefits for those enrolled in both Medicare and Medicaid, known as dual eligibles, can be complicated. New Jersey offers integrated programs streamlining care coordination for dual-eligible individuals. This simplifies access to services and maximizes benefits from both programs, minimizing potential gaps in coverage.
Spend-Down Provisions: Bridging the Gap
If your income is slightly above the standard Medicaid limits, spend-down provisions can help you qualify. Spend-down allows you to allocate excess income towards medical expenses to reach the eligibility threshold. This option offers critical assistance for those facing high medical costs, ensuring they can still access vital healthcare.
By exploring these specialized programs, you can gain a complete understanding of the full scope of Medicaid benefits available in New Jersey. Whether you need long-term support, help with nursing home costs, or prefer community-based care, understanding these programs empowers you to find the appropriate coverage for your unique circumstances. For more information on senior care resources and Medicaid eligibility in New Jersey, visit Caring Hands Senior Services.
Keeping Your Coverage: Renewals and Redeterminations
Securing Medicaid eligibility in New Jersey is a big step towards accessible healthcare. But keeping that coverage requires ongoing attention. This section offers essential guidance on navigating the renewal process, ensuring you maintain your NJ FamilyCare benefits without interruption.
Understanding Redeterminations: How Often Does It Happen?
Medicaid eligibility isn't permanent. Regular redeterminations, also called renewals, assess if you still qualify for the program. These typically happen annually. However, the exact timing depends on individual circumstances and program updates. Knowing your specific renewal date is crucial.
The Renewal Process: What to Expect and How to Prepare
NJ FamilyCare will notify you when it's time for your redetermination. This notice usually arrives by mail, though some people receive electronic notifications. Pay close attention to these notices, as they have important information and deadlines.
The renewal process involves updating your information with NJ FamilyCare. You’ll need to provide current details about your household size, income, and any other relevant changes. Gathering necessary documents, like proof of income and residency, beforehand can simplify the process.
Reporting Changes Between Renewals: Staying Proactive
Even if your annual renewal isn't due yet, certain life changes must be reported to NJ FamilyCare. These changes include:
- Income Changes: Report significant income increases or decreases promptly, as they directly affect your eligibility.
- Household Changes: Report changes in household size, such as births, deaths, or people moving in or out.
- Address Updates: Keep NJ FamilyCare informed of any address changes to ensure you receive important notices.
You can report these changes online through the NJ FamilyCare portal, by phone, or by mail. Using the right reporting methods ensures your information is processed correctly and efficiently.
Common Reasons for Coverage Loss: And How to Avoid Them
Many people lose Medicaid coverage unexpectedly because of avoidable mistakes. Here are some common reasons:
- Missing Renewal Deadlines: Failing to complete and submit renewal paperwork on time is a major cause of coverage loss.
- Not Reporting Changes: Neglecting to report changes in income or household can lead to ineligibility.
- Incorrect or Incomplete Information: Providing inaccurate or incomplete information during the application or renewal process can put your coverage at risk.
By understanding these common issues, you can take proactive steps to keep your Medicaid eligibility. Staying organized, meeting deadlines, and reporting changes promptly are key to avoiding unexpected gaps in coverage.
Understanding Your Appeal Rights: What to Do If Coverage Is Terminated
If your Medicaid coverage ends, you have the right to appeal the decision. This process allows you to present your case and possibly regain your benefits. Understand the steps involved and deadlines for filing an appeal. Getting help from an enrollment counselor or legal aid organization can be invaluable. They can offer personalized support and ensure your appeal is filed correctly.
For personalized care, contact Caring Hands Senior Services. We provide in-home care for seniors and individuals with disabilities in Mercer County, New Jersey. Our services include personal care, nursing services, respite care, and companionship, helping individuals maintain independence and quality of life at home.